Medicine and Health
A microphysiological system for studying barrier health of live tissues in real time
R. Way, H. Templeton, et al.
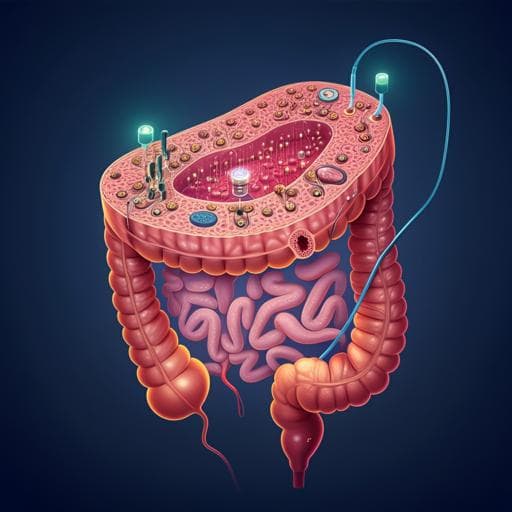
The intestinal epithelial barrier is essential for maintaining homeostasis, and its disruption ("leaky gut") is implicated in disorders such as inflammatory bowel disease and neurodegenerative conditions. Real-time assessment of barrier integrity is commonly performed via transepithelial/transendothelial electrical resistance (TEER). However, conventional TEER approaches using simplified in vitro monolayers (e.g., Transwells) or even organ-on-a-chip (OoC) devices lack the cellular complexity of intact tissues, while classic ex vivo Ussing chambers are bulky, use static media, and typically maintain viability for less than 3 hours. The research question addressed here is whether an integrated microphysiological platform can preserve the complex, intact mouse colon barrier ex vivo under physiologic-like conditions for extended durations, while enabling real-time, repeatable TEER measurements to quantify barrier changes under controlled perturbations. The study aims to maintain oxygen gradients and microbiome-supportive conditions, deliver microfluidic flow to extend viability, and integrate electrodes/electronics for continuous TEER and impedance spectroscopy, thereby bridging the gap between physiologic fidelity and quantitative barrier monitoring.
Existing methods to interrogate epithelial barrier integrity include dye-based paracellular flux and TEER. Transwells with chopstick electrodes offer simplicity and throughput but lack physiological flow and show variability. Organs-on-chips add microfluidics and mechanical cues, improving environmental control but still lack the full cellular and structural diversity of intact tissue. Classical Ussing chambers established electrical measurements for transport and permeability but are limited by static media, low throughput, bulky benchtop equipment, and short ex vivo viability (<3 h). Recent ex vivo microfluidic devices improved viability (often >48 h) by delivering flow and tailored media (including oxygen gradients) but generally lack real-time TEER, requiring destructive time points and more animals. Prior devices with TEER often use external benchtop instruments and stick electrodes, with limited frequency ranges and minimal integration. The presented system builds on these advances by integrating microfluidics, physiologically relevant media (including microbiome-supportive components and oxygen gradients), on-chip electrodes, and custom electronics for real-time TEER/EIS in intact colon tissue over extended periods.
Microfluidic chamber design: Chambers were CAD-designed and SLA-printed in UV-curable resin, fully UV-cured and IPA-rinsed, and sterilized (including low-temperature autoclave for metal parts). Each chamber comprises two halves: chamber body, PDMS layers (for sealing and holding the electrode chip), a gold electrode chip on glass, an aluminum clamp, and PCB boards with spring headers for electrical contact. The top half includes tissue-holding spikes around the periphery; a PDMS layer ensures a flush seal. The tissue is positioned over a circular aperture forming a barrier between luminal and serosal microfluidic pathways, with uniform flow achieved by CFD-guided channel design. Chambers are oriented vertically during operation to facilitate bubble removal.
Microfluidics and operation: Luer-lock tubing connects to each half; custom syringe pumps deliver media with programmable timing. At experiment start, a purge at 25,000 μL/h for 45 s removes bubbles, then flow is maintained at 250 μL/h per side. Effluent is collected to verify balanced outflow. Chambers, media, and electronics are housed at 37 °C in an incubator.
System overview and electronics: The system resides in a shielded metal enclosure with USB connectivity and supports up to three chambers simultaneously via card-edge connectors. Custom GUI software controls experiments and displays TEER in real time. TEER measurement uses a constant-current approach. A USB FTDI module interfaces with onboard control electronics. A signal generator drives a Howland current source (HCS) to supply AC current to electrodes. Read channels include a transimpedance amplifier (TIA) for current and an instrumentation amplifier (INA) for voltage. Relays discharge electrode charge buildup to prevent saturation/drift. Level shifting stages and digitally controlled potentiometers are used to center signals within ADC range; the potentiometers are auto-calibrated (binary search) to minimize DC offset. The system’s electronics are split into a main control board (power supplies, microcontroller, ADC, signal generators, control level shifters) and a TEER acquisition board (HCS blocks, read channels, calibration elements, chamber connectors). Architecture is designed to be scalable.
Electrode design and fabrication: Gold electrodes on a 25 × 25 mm glass substrate form a 4-point configuration: an outer ring current electrode and a central voltage-sensing electrode. Fabrication used in-house photolithography, metal deposition, and lift-off with a custom mask.
Sterilization: All chamber components underwent: 20 min in 1:10 bleach, ultrasonic soapy water bath (10 min), DI water rinse, 45 min in 70% ethanol, DI rinses, air dry, assembly with autoclaved clamps/screws, followed by low-temperature gas sterilization and sealed storage.
Animals and tissue preparation: Male C57BL/6 mice (3–4 months) were used under IACUC-approved protocols. Intestines were removed post-decapitation and placed in 4 °C Krebs buffer (with nicardipine to prevent contractions). Colon was dissected; in some cases, the muscularis externa was teased away with a 26 G needle. Tissue was cut longitudinally into ~5 mm flat pieces.
Media: Custom Adult Neurobasal-based media with 2% B27, 4 mM glucose, and 3% HEPES (no phenol red). Luminal media included 0.4 mg/mL inulin and sodium sulfite as an oxygen scavenger to lower luminal O2, while serosal media remained at ambient O2, creating an oxygen gradient to preserve microbiome. After 24 h, control luminal media were not changed. Treatments: luminal collagenase (5.80×10^2 U) or acidified media (HCl, pH 2) applied from 24–48 h.
Histology: After experiments, tissues were protected with CPC in PBS, fixed in 4% PFA + 0.5% CPC at 4 °C for 24 h, stored in PBS, embedded in agarose, and sectioned at 50 μm. Lectin (UEA-1 rhodamine) labeled goblet cell mucopolysaccharides; immunohistochemistry used anti-claudin-1 and anti-peripherin with fluorescent secondary antibodies. Imaging used confocal and brightfield microscopes. Toluidine blue staining confirmed muscle dissection.
TEER calculation and EIS: For each measurement, a sinusoidal current (85 μA) was swept from 12 Hz to 5 kHz across 20 frequencies; square-wave stimuli were also applied. Signals underwent drift correction (subtracting a first-order polynomial) and sinusoidal curve fitting to extract magnitude and phase for voltage and current, yielding impedance spectra. TEER was derived from magnitude |Z| at an appropriate frequency (~5 kHz) after subtracting baseline media/electrode contributions. Square-wave responses provided resistive components less affected by electrode double-layer capacitance. Measurements were taken every 2 h over 48 h; the first ~24 h were considered a calibration/equilibration period.
Viability assessment: Separate viability studies maintained tissues under continuous control flow up to 72 h, with histological evaluation of mucosal architecture, goblet cells, and tight junctions (claudin-1) to confirm barrier integrity.
- System electrical performance: The read-channel bandwidth was limited by the TIA to 47.5 kHz, approximately 10× the maximum stimulus frequency (5 kHz), ensuring minimal attenuation of TEER signals while filtering high-frequency noise. Noise PSD measurements yielded total noise power of 0.126 μV^2 and SNR of 28.14 dB; ADC sampling at 806.4 ksps with 12-bit resolution. The system’s impedance measurement range with <5% error was 150–6.5 kΩ. The HCS DC offset current was 1.87 μA. Step responses showed stable, non-ringing behavior.
- Stimulus waveform effects: TEER from square-wave stimuli was on average 7.2% lower than TEER from 5 kHz sinusoidal stimuli (n=10), consistent with reduced influence of electrode double-layer capacitance during rapid transitions. The percent difference increased as sinusoidal frequency decreased and plateaued for ≥3 kHz, indicating higher frequencies mitigate double-layer effects.
- Tissue viability: Colon explants maintained intact mucosal, submucosal, and muscular layers with preserved crypt patterning after 72 h. Goblet cells retained morphology comparable to in vivo controls, and apical goblet cell counts in the upper third of crypts showed no significant difference between in vivo and 72 h ex vivo tissues. Claudin-1 immunoreactivity remained around epithelial cells after 72 h, indicating preserved tight junction integrity.
- Barrier disruption detected by TEER and histology: Collagenase treatment from 24–48 h caused progressive TEER reductions correlated with goblet cell rounding and moderate decreases in claudin-1 immunoreactivity, indicating increased permeability. Acidic luminal media (pH 2) produced pronounced TEER decreases and marked epithelial damage, including sloughing and dramatic loss of claudin-1 signal.
- Sensitivity to tissue composition and location: Removing the muscularis externa decreased settled TEER (after ~24 h equilibration) by about 39%, aligning with literature that subepithelial resistance contributes variably (15–80%) to total resistance depending on intestinal region and species. Toluidine blue staining confirmed complete muscle removal. TEER also differed by colon region, with distal colon showing ~19% lower settled TEER than proximal colon (proximal n=9, distal n=6; significance reported as P<0.01). Muscle-intact n=15; cut-muscle n=7; P<0.005 reported.
- System capabilities: The platform simultaneously supports up to three chambers, provides programmable microfluidic flow, and acquires real-time TEER/EIS (12 Hz–5 kHz) at user-defined intervals, enabling longitudinal monitoring over 48 h and viability up to 72 h.
The system addresses the central need for a physiologically relevant ex vivo model that retains intact tissue complexity while enabling real-time, quantitative assessment of barrier integrity. By maintaining oxygen gradients and microbiome-supportive conditions under controlled microfluidic flow, the platform preserved colon tissue viability and tight junction function for up to 72 h, surpassing the typical limitations of Ussing chambers. Integrated electrodes and custom electronics enabled stable, repeatable TEER/EIS measurements over 48 h and captured dynamic barrier changes in response to defined luminal insults (collagenase, low pH). The concordance between TEER reductions and histological indicators (goblet cell morphology changes and decreased claudin-1) validates TEER as a functional readout of barrier impairment in intact tissue. The ability to detect differences due to subepithelial structures (muscle removal) and anatomical location (proximal vs distal) demonstrates sensitivity to physiological heterogeneity and aligns with prior literature on subepithelial contributions to transmural resistance. The compact, scalable, multi-chamber design and GUI-controlled operation facilitate parallel experiments and reduce the need for multiple animals and destructive time points, potentially accelerating studies in gut barrier physiology, disease modeling, and preclinical testing.
This work introduces a compact, integrated microphysiological system that sustains ex vivo mouse colon viability while enabling real-time TEER/EIS measurements. Key contributions include: (1) a dual-flow microfluidic chamber and tailored media that preserve microbiome and oxygen gradients to maintain barrier health up to 72 h; (2) integrated gold electrodes with custom electronics and software for stable, drift-corrected TEER/EIS over 12 Hz–5 kHz with measurements every 2 h; and (3) demonstration of biological relevance through correlation of TEER with histological markers and sensitivity to tissue composition and anatomical region. The system reduces reliance on bulky benchtop equipment, fits within an incubator, and is scalable to multiple simultaneous samples. Potential future directions include adapting the chamber geometry and media for other barrier tissues (e.g., esophagus, skin, airway), integrating additional sensing modalities (e.g., optical, metabolic, cytokine sensors), expanding channel count for higher throughput, and applying the platform to human tissues for translational studies and drug testing.
- TEER time-series were analyzed primarily over 24–48 h; the first ~24 h showed equilibration-related variability, and exposures such as low pH led to degradation that limited longer TEER tracking, although histological viability was demonstrated at 72 h.
- Measurement fidelity depends on frequency selection due to electrode double-layer capacitance; TEER values are frequency-dependent at low frequencies and require baseline subtraction and drift correction.
- The validated impedance range with <5% error (150–6.5 kΩ) constrains optimal operating conditions; accuracy may decrease outside this range.
- Demonstrations were performed on mouse colon; generalization to other tissues and species (including human) remains to be empirically validated, though the design is adaptable.
- Data and custom code are available upon request rather than publicly posted, which may impact immediate reproducibility.
- Sample sizes for some comparisons were modest (e.g., muscle removal n=7 vs n=15; proximal n=9 vs distal n=6), though statistical significance was reported.
Related Publications
Explore these studies to deepen your understanding of the subject.







