Medicine and Health
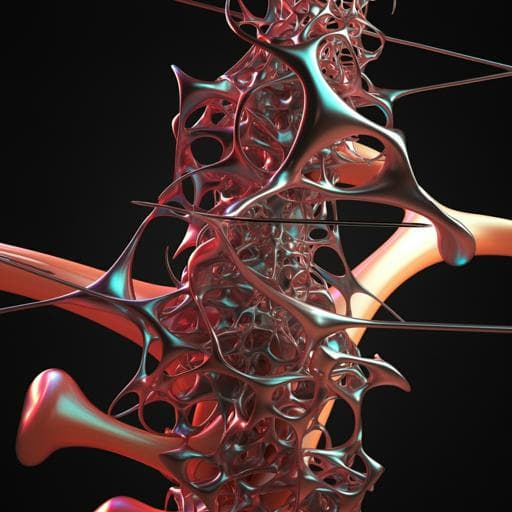
A biomimetic engineered bone platform for advanced testing of prosthetic implants
M. Sladkova-faure, M. Pujari-palmer, et al.
This groundbreaking research conducted by authors like Martina Sladkova-Faure and Michael Pujari-Palmer explores an innovative biomimetic human bone platform for testing prosthetic implants. The study reveals how titanium implants outperform stainless steel in integration and mineralization, challenging traditional testing methods and paving the way for more relevant outcomes in implant osseointegration.
Related Publications
Explore these studies to deepen your understanding of the subject.