Medicine and Health
Trastuzumab deruxtecan versus trastuzumab emtansine in HER2-positive metastatic breast cancer: long-term survival analysis of the DESTINY-Breast03 trial
J. Cortés, S. A. Hurvitz, et al.
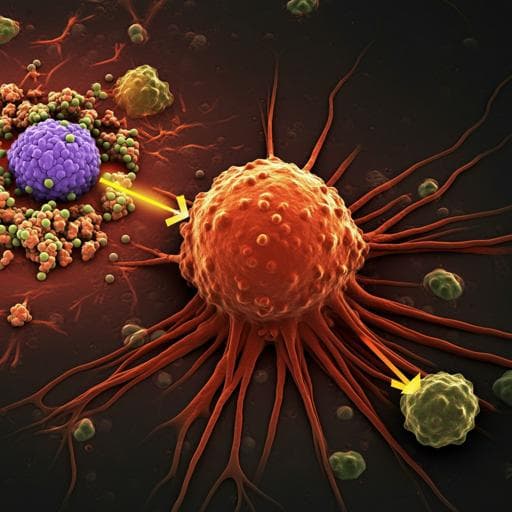
Human epidermal growth factor receptor 2 (HER2)-positive breast cancer is characterized by amplification of the HER2 (ERBB2) gene and/or overexpression of the HER2 protein, driving aggressive tumor behavior and affecting about 20% of breast cancers. Targeted HER2 therapies have improved prognosis in this subtype. Trastuzumab deruxtecan (T-DXd) is approved in multiple regions for HER2-positive metastatic breast cancer after prior taxane and trastuzumab or early recurrence post-(neo)adjuvant therapy and is guideline-recommended. DESTINY-Breast03 is a multicenter phase 3 trial comparing T-DXd with trastuzumab emtansine (T-DM1), previously the standard in this setting. Both agents are HER2-directed antibody-drug conjugates with different payloads and linkers; T-DXd uses a topoisomerase I inhibitor with a cleavable linker and has a higher drug-to-antibody ratio (~8 vs ~3.5 for T-DM1). The primary endpoint was PFS by blinded independent central review (BICR), with a key secondary endpoint of OS. Earlier analyses showed significant PFS benefit and OS improvement with T-DXd versus T-DM1, though median OS was previously unreached. Following the significant PFS findings, further BICR tumor response assessment was discontinued. This report provides an exploratory updated analysis (data cutoff 20 November 2023) with longer follow-up, reporting updated efficacy including median OS and safety.
Design and participants: DESTINY-Breast03 (NCT03529110) is an open-label, multicenter, randomized phase 3 trial comparing T-DXd (5.4 mg/kg IV every 3 weeks) versus T-DM1 (3.6 mg/kg IV every 3 weeks) in patients with HER2-positive, unresectable or metastatic breast cancer previously treated with trastuzumab and a taxane. Randomization was 1:1 using balanced blocks, stratified by hormone receptor status, prior pertuzumab, and history of visceral disease via a web-based system. Due to differing administration and AE profiles, the trial was open-label; earlier tumor assessments for the primary analysis were conducted by BICR.
Eligibility: Adults with centrally confirmed HER2-positive disease (IHC 3+ or IHC 2+ with positive in situ hybridization), prior trastuzumab and taxane in advanced/metastatic settings or progression within 6 months of (neo)adjuvant therapy; measurable disease with radiologic progression; adequate renal/hepatic function. Key exclusions included significant/uncontrolled cardiovascular disease (e.g., recent MI, symptomatic heart failure, prolonged QT, abnormal troponin, LVEF <50% within 28 days), prior HER2-directed ADC, and history of noninfectious ILD/pneumonitis requiring steroids or active/uncertain ILD/pneumonitis. Patients with inactive/asymptomatic brain metastases not requiring corticosteroids/anticonvulsants or recovered from radiotherapy were eligible; at least 2 weeks were required after whole-brain radiotherapy before enrollment.
Assessments and procedures: Baseline assessments preceded first dose; visits occurred on day 1 of each 21-day cycle, with additional day 8 and 15 assessments in cycle 1. Tumor assessments were scheduled every 6 weeks from randomization. End-of-treatment assessments were within 7 days of discontinuation, with a follow-up at 40 days post-treatment or before new anticancer therapy; long-term follow-up every 3 months continued until death, consent withdrawal, loss to follow-up, or study closure. Suspected ILD/pneumonitis events were reviewed by an external independent adjudication committee. AEs were graded per CTCAE v5.0 and coded with MedDRA v25.0.
Endpoints: Primary endpoint was PFS by BICR (reported previously). The key secondary endpoint was OS. Other secondary/exploratory endpoints in this report included ORR, DoR, PFS, and PFS2 by investigator assessment, and safety. PFS2 was defined as time from randomization to progression on the next line of therapy or death; the next line was the first new systemic antineoplastic therapy after discontinuation of study treatment.
Statistical analysis: Efficacy analyses were conducted on the full analysis set (all randomized). Safety analyses included all randomized patients who received ≥1 dose (safety analysis set). Time-to-event endpoints (PFS, OS, PFS2, DoR) used Kaplan–Meier methods with medians and 95% CIs (Brookmeyer–Crowley) and stratified log-rank tests according to randomization factors; HRs with 95% CIs used stratified Cox models. ORR was analyzed using Cochran–Mantel–Haenszel tests with stratification factors and Clopper–Pearson 95% CIs. A hierarchical testing plan allowed OS testing after PFS significance; the updated OS analysis here is exploratory because significance was met at the second OS interim analysis. Sensitivity analysis for OS employed a rank-preserving structural failure time model (RPSFTM) with recensoring to adjust for post-trial T-DXd in the T-DM1 arm (estimated acceleration factor exp() = 0.425). Software included SAS (v9.3+) and R (4.2.0) for RPSFTM.
Oversight and ethics: The study was designed by Daiichi Sankyo and conducted per the Declaration of Helsinki, ICH-GCP, local regulations, and protocol, with ethics/IRB approval at each site. All patients provided written informed consent. No patient compensation was provided.
- Population: 699 screened; 524 randomized (T-DXd n=261; T-DM1 n=263). Median age ~54 years; ECOG 0/1 in majority; HER2 IHC 3+ in ~89%; baseline CNS metastases in ~16% (T-DXd) and ~15% (T-DM1). Median prior metastatic therapy lines: 2 in both arms. As of 20 Nov 2023, 19.5% (T-DXd) vs 3.8% (T-DM1) remained on treatment; median follow-up 43.0 vs 35.4 months.
- Efficacy (investigator assessment): • Objective response rate: 78.9% (206/261; 95% CI 73.5–83.7) with T-DXd vs 36.9% (97/263; 95% CI 31.0–43.0) with T-DM1; complete responses 12.6% vs 4.2%; partial responses 66.3% vs 32.7%. • Duration of response (median): 30.5 months (95% CI 23.0–NE) with T-DXd vs 17.0 months (95% CI 14.1–23.7) with T-DM1; DoR rate at 36 months 48.9% vs 28.7%. • Progression-free survival (median): 29.0 months (95% CI 23.7–40.0) with T-DXd vs 7.2 months (95% CI 6.8–8.3) with T-DM1; HR 0.30 (95% CI 0.24–0.38). PFS rates: 24 months 55.8% vs 12.4%; 36 months 45.7% vs 20.6%; 48 months 41.5% vs 9.9%. • PFS2 (median): 45.2 months (95% CI 39.3–NE) with T-DXd vs 23.1 months (95% CI 17.8–29.7); HR 0.53 (95% CI 0.41–0.68); 36-month PFS2 rates 62.1% vs 40.3%. • Overall survival: 236 OS events (T-DXd 110 [42.1%]; T-DM1 126 [47.9%]). Median OS 52.6 months (95% CI 48.7–NE) with T-DXd vs 42.7 months (95% CI 35.4–NE) with T-DM1; HR 0.73 (95% CI 0.56–0.94). OS rates: 24 months 77.5% vs 70.1%; 36 months 67.6% vs 55.7%; 48 months 56.9% vs 48.3%. • Sensitivity (RPSFTM) adjusting for post-trial T-DXd in T-DM1 arm: adjusted median OS 39.8 months (95% CI 32.4–NE) for T-DM1; HR for OS T-DXd vs adjusted T-DM1 0.66 (95% CI 0.51–0.87).
- Post-trial therapy among those who discontinued study treatment: 69.6% (T-DXd) and 78.9% (T-DM1) received systemic therapy; 52.1% of T-DXd arm received T-DM1; 32.3% of T-DM1 arm received T-DXd.
- Safety: • Median treatment duration: 18.2 months (range 0.7–56.6) T-DXd vs 6.9 months (0.7–55.2) T-DM1. • Any-grade TEAEs: 99.6% vs 95.4%; Grade ≥3 TEAEs: 58.0% vs 52.1%; serious TEAEs: 27.6% vs 22.6%. • Drug-related discontinuations: 22.6% (T-DXd) vs 7.3% (T-DM1); most common with T-DXd: pneumonitis 6.6% and ILD 5.4%; with T-DM1: pneumonitis 1.5% and platelet count decreased 1.5%. • Dose reductions due to drug-related TEAEs: 28.0% vs 15.3%; drug interruptions: 44.0% vs 18.4%. • Exposure-adjusted incidence rates (per patient-year): any-grade TEAEs 0.53 (T-DXd) vs 1.10 (T-DM1); Grade ≥3 TEAEs 0.31 vs 0.60; serious TEAEs 0.15 vs 0.26. • Adjudicated drug-related ILD/pneumonitis (any grade): 16.7% (T-DXd; grade 1: 4.3%, grade 2: 11.7%, grade 3: 0.8%) vs 3.4% (T-DM1; grade 1: 1.9%, grade 2: 1.1%, grade 3: 0.4%); no grade 4/5 events. Four new grade 2 ILD events with T-DXd since prior cutoff; most occurred during year 3 (time to onset 832–961 days). EAIRs: 0.09 (T-DXd) vs 0.04 (T-DM1). • LVEF decrease/left ventricular dysfunction: 4.3% (T-DXd) vs 1.5% (T-DM1); EAIR 0.02 for both; no new high-grade signals.
- Overall, T-DXd showed sustained and superior efficacy versus T-DM1 with manageable and consistent safety over longer follow-up.
This updated analysis of DESTINY-Breast03 demonstrates that T-DXd confers durable and clinically meaningful benefits over T-DM1 in previously treated HER2-positive metastatic breast cancer. Investigator-assessed median PFS with T-DXd was about four times that with T-DM1, and nearly half of T-DXd–treated patients remained progression free at 3 years. ORR was substantially higher and responses more durable with T-DXd. Median OS was reached for both arms, showing an approximately 10-month improvement and a 27% reduction in risk of death with T-DXd versus T-DM1; sensitivity analyses adjusting for post-trial T-DXd in the T-DM1 arm suggested an even larger OS benefit. While cross-trial comparisons warrant caution, the observed PFS and OS with T-DXd compare favorably with historical outcomes in this disease setting, underscoring potential advantages of earlier T-DXd use. Safety findings remained consistent with prior reports, with higher rates of treatment modifications in the T-DXd arm but lower exposure-adjusted incidence rates versus T-DM1 due to longer treatment duration. ILD/pneumonitis events with T-DXd were mostly grade 1–2, occurred predominantly within the first year, with a few new grade 2 events emerging in year 3, and no grade 4/5 events, supporting ongoing monitoring and prompt management. Collectively, these results reinforce T-DXd as a superior option over T-DM1 in this setting.
With extended follow-up, T-DXd maintained superior efficacy over T-DM1 in HER2-positive metastatic breast cancer previously treated with taxane and trastuzumab, delivering the longest median OS reported to date in this setting (52.6 months) alongside marked improvements in PFS, PFS2, ORR and DoR, and a manageable safety profile without new safety signals. These findings support the use of T-DXd earlier in the treatment sequence. Future work includes continued follow-up for more mature OS data, analyses of long-term responders across studies, and trials exploring T-DXd in earlier metastatic settings (e.g., DESTINY-Breast09).
This updated analysis was exploratory. PFS, ORR and DoR were assessed by investigators rather than BICR, and no formal statistical comparisons were made for these endpoints. Although an OS HR favored T-DXd, the current OS analysis was exploratory as statistical significance had already been established at a prior interim analysis; additional follow-up is needed to refine the median OS estimate in the T-DXd arm due to censoring. Cross-trial comparisons cited are indirect and subject to differences in study design and post-trial therapies.
Related Publications
Explore these studies to deepen your understanding of the subject.