Medicine and Health
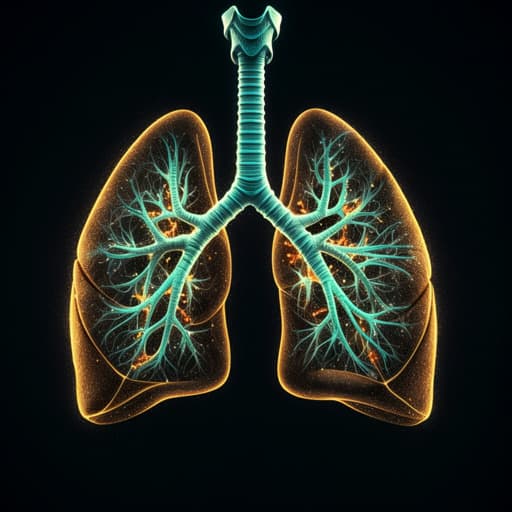
The Long Run towards Personalized Therapy in Non-Small-Cell Lung Cancer: Current State and Future Directions
C. Genova
Explore the latest advancements and ongoing challenges in personalized therapy for non-small-cell lung cancer (NSCLC) as discussed by Carlo Genova. This insightful editorial delves into the complexity of NSCLC treatment, including the rise of targeted therapies and the fascinating role of artificial intelligence in enhancing personalized medicine.
Related Publications
Explore these studies to deepen your understanding of the subject.