Medicine and Health
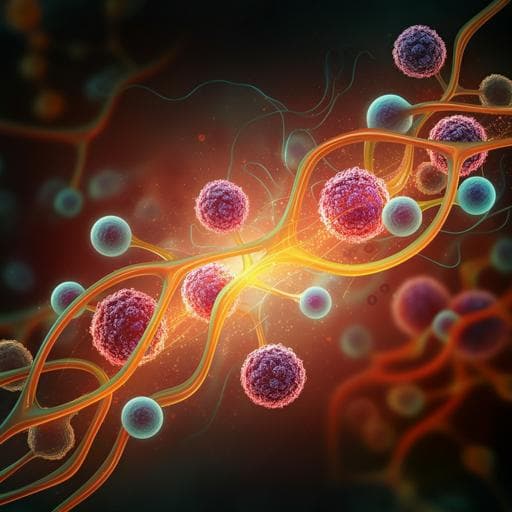
Sulforaphane alleviates psoriasis by enhancing antioxidant defense through KEAP1-NRF2 Pathway activation and attenuating inflammatory signaling
C. Ma, C. Gu, et al.
Discover the remarkable effects of sulforaphane on psoriasis in this groundbreaking study conducted by Chujun Ma and colleagues. The treatment not only alleviated symptoms but also revealed powerful molecular mechanisms that activate the KEAP1-NRF2 pathway, showcasing sulforaphane's potential as a therapeutic agent.
Related Publications
Explore these studies to deepen your understanding of the subject.