Medicine and Health
Stratified Functional Analysis of Bacterial Genes Associated With Pulmonary Exacerbations in Cystic Fibrosis
A. Hahn, E. Córdoba-lanús, et al.
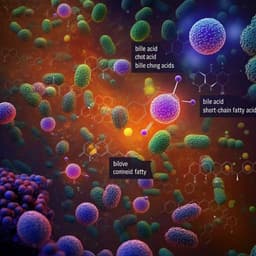
Cystic fibrosis (CF) is a genetic disease driven by CFTR dysfunction, leading to impaired mucociliary clearance, chronic airway infections, and inflammation. Acute declines in lung function and health status, termed pulmonary exacerbations (PEx), often require antibiotic interventions. Given heterogeneity in CF genotypes/phenotypes and the limits of treatments targeted solely at pathogens or host factors, characterizing changes in the airway microbiome and metabolome across clinical states may offer additional insight. This study aimed to perform a stratified functional analysis of bacterial genes across three clinical states—PEx hospitalization, end of antibiotic treatment, and follow-up—to determine roles of specific microbiome members within each state. A secondary goal was to compare changes between clinical states with the metabolic activity of specific microbiome members. The hypothesis was that differences in gene expression of specific community members are detectable between clinical states and correlate with differences in metabolic activity, providing insight into mechanisms underlying clinical changes and microbial contributions.
Design: Single-center, prospective observational study at Children’s National Hospital (Washington, DC) from 2016–2020, enrolling persons with CF treated with intravenous antibiotics for pulmonary exacerbation (PEx). IRB approvals Pro6781 and Pro10528; informed consent/assent obtained. Participants could re-enroll with subsequent exacerbations. Time points: Samples and clinical data collected at PEx onset (start of IV antibiotics), end of antibiotic treatment, and follow-up (adapted from BETR criteria). Specimens: Sputum, oropharyngeal swab (OP), or bronchoalveolar lavage (BAL) collected clinically. Processing: Samples kept at 4°C until processing. For metagenomics, sputum/BAL mixed with Sputasol and saline, homogenized (37°C bead bath), centrifuged (12,000 g, 10 min) to pellet cells; supernatants and pellets stored at −80°C. OP swab Amies media processed similarly. Clinical microbiology cultures performed. DNA extraction and sequencing: Bacterial DNA extracted using QIAamp DNA Microbiome Kit. DNA quantity (Qubit) and quality (Bioanalyzer) assessed. Libraries prepared with Nextera XT and sequenced on Illumina NextSeq 500 (Mid-Output 2 × 150), 20–30 libraries/run. ZymoBiomics Microbial Community Standards included as controls. Bioinformatics: Quality control with FastQC; trimming with Flexbar. Human read removal with KneadData. Taxonomic profiling with MetaPhlAn3 (“rel_ab_w_read_stats” for count tables). Functional profiling with HUMAnN3 for genes, pathways, and taxa contributions; pathways from MetaCyc; Gene Ontology (GO) regrouping via humann_regroup. Statistics: Relative abundance and count tables analyzed in R (DESeq2 v1.24.0 for differential abundance with log fold change shrinkage; ggplot2; phyloseq; vegan). Alpha diversity (species observed, Shannon, inverse Simpson) computed; beta diversity assessed with Bray-Curtis and PERMANOVA (adonis), controlling for repeated measures via strata. STATA/IC v15.1 used for additional statistical comparisons across time points. Sensitivity: Prior analysis indicated congruence across sample types; no adjustment for sample type in main analyses. Sequencing controls showed strong correlation with expected compositions (R 0.743–0.812; R2 0.552–0.659; all p < 0.01).
Cohort: 22 participants (45 PEx); median age 16.5 y (range 7–23), 41% female; 68% had ≥1 F508del allele. CFTR modulators at 42% of PEx (ivacaftor n=5, ivacaftor/lumacaftor n=12, tezacaftor/ivacaftor n=2). Baseline at first PEx: BMI 19.4 (SD 3.5), best ppFEV1 in prior 6 months 81.4% (SD 25.9%). Cultures during PEx commonly grew Pseudomonas aeruginosa (47%), MRSA (20%), MSSA (16%). Antibiotics commonly used: tobramycin (62%), ceftazidime (36%), meropenem (27%); median course 14–15 days. Lung function: ppFEV1 improved from PEx to end of treatment (65.1 vs. 80.3, p < 0.001; 42/45 observed), and differed between end of treatment and follow-up (80.4 vs. 70.5, p < 0.001; 41/45 observed). Sequencing/communities: 34 PEx, 33 end-of-treatment (2 failed, 10 not collected), 39 follow-up samples sequenced; total of 211 bacterial species identified; 1–86 species/sample. Alpha diversity: No significant differences between PEx and end-of-treatment; significant increases from end-of-treatment to follow-up (species observed p < 0.001; Shannon p = 0.047; inverse Simpson p = 0.020). Beta diversity: Significant differences across time points (PERMANOVA p = 0.001), driven by end-of-treatment shift. Differential taxon abundance: Only Gemella haemolysans increased in PEx vs. end-of-treatment (log2FC 4.7, padj < 0.001). In follow-up vs. end-of-treatment, Gemella haemolysans (log2FC 5.0, padj < 0.001) and Streptococcus salivarius (log2FC 5.1, padj = 0.004) increased. Differential gene abundance (HUMAnN3, GO categories): 10 species (≈4.5%) showed significant differential gene abundance across clinical states (padj < 0.01; |log2FC| > 2): Gemella haemolysans, Gemella morbillorum, Neisseria flavescens, Staphylococcus argenteus, Staphylococcus aureus, Streptococcus mitis, Streptococcus oralis, Streptococcus salivarius, Veillonella atypica, Actinomyces sp. oral taxon 181. PEx vs. end-of-treatment: 1,608 genes significant (BP 552; MF 951; CC 83; 22 uncategorized), with Staphylococcus aureus accounting for ~81% (1,306 genes). Follow-up vs. end-of-treatment: 989 genes significant (BP 358; MF 566; CC 50; 15 uncategorized), with Streptococcus salivarius accounting for ~83% (821 genes). Unique genes: 673 genes unique to PEx (651 S. aureus); 128 unique to follow-up (121 S. salivarius). Follow-up vs. PEx: 11 genes (all Veillonella atypica) significant across GO categories (log2FC ~2.5–3.5). Differential metabolic pathways: 8,653 pathways identified; 120 significantly differentially abundant overall (|log2FC| > 2). PEx vs. end-of-treatment: 106 significant pathways, all in Staphylococcus aureus; 53 unique to PEx across 16 of 17 MetaCyc superfamilies, notably “Cofactor, prosthetic group, electron carrier, and vitamin biosynthesis” (18 pathways) and “Nucleotide and nucleoside biosynthesis” (8 pathways). Follow-up vs. end-of-treatment: 66 significant pathways, all in Streptococcus salivarius; 13 unique pathways across 4 superfamilies, most in carbohydrate biosynthesis (4) and carbohydrate degradation (3). Follow-up vs. PEx: only one significant pathway, in Veillonella atypica—UDP-N-acetyl-D-glucosamine biosynthesis I (carbohydrate biosynthesis).
The study supports that relatively few species (~5%) drive functional shifts across CF clinical states, with pronounced roles for Staphylococcus aureus during PEx and Streptococcus salivarius during follow-up. The dominance of S. aureus gene and pathway changes at PEx suggests metabolic adaptations to the nutrient-limited, inflamed CF airway that may promote persistence and antimicrobial tolerance, including enrichment of cofactor/vitamin and nucleotide biosynthesis pathways linked to bacterial survival and pathogenesis. In contrast, follow-up is characterized by functional activity from S. salivarius, whose role can be context-dependent but has been associated with comparatively milder disease than classic CF pathogens. A key observation is the specific involvement of Veillonella atypica when comparing follow-up to PEx: only V. atypica harbored differentially abundant genes and a single pathway (UDP-N-acetyl-D-glucosamine biosynthesis I), producing GlcNAc, a metabolite implicated in activating glycolysis and peptidoglycan biosynthesis. Given prior associations of Veillonella with milder CF disease and its relative absence of differential activity during PEx, these data point to potentially beneficial community interactions involving anaerobes like V. atypica that may relate to recovery of lung function post-treatment. Overall, functional metagenomic readouts (genes and metabolic pathways) provided clearer insights into clinical state transitions than taxonomic relative abundance alone.
Approximately 5% of observed bacterial species exhibited differential gene abundance across clinical states in CF, with three species—Staphylococcus aureus (PEx), Streptococcus salivarius (follow-up), and Veillonella atypica (follow-up vs. PEx)—accounting for most functional changes. Metabolic pathways enriched during PEx, particularly in S. aureus, implicate biosynthetic capacities that may underlie exacerbation-associated inflammation and persistence. The singular V. atypica pathway difference (UDP-N-acetyl-D-glucosamine biosynthesis I) between follow-up and PEx suggests anaerobe-linked metabolites could contribute to improved lung function. These findings indicate that metabolic potential and functional activity of airway microbiome members may be more informative for understanding clinical state transitions than taxonomic abundance alone. Future work should validate these findings in larger, multi-center, longitudinal cohorts and assess whether specific microbial functional markers can predict impending exacerbations or guide targeted therapies.
- Single-center study focused on children and young adults capable of producing sputum at PEx onset; small sample size and potential bias toward more symptomatic individuals limit generalizability. - Sampling centered around a single PEx episode per enrollment rather than extended longitudinal tracking, limiting ability to evaluate temporal dynamics and predictive value of functional markers. - Some samples were not collected or failed sequencing at certain time points, reducing paired comparisons. - Heterogeneous sample types (sputum, OP swab, BAL) were not adjusted for in analyses, though prior sensitivity analyses suggested congruence. - Metagenomic functional inferences rely on reference databases and may not capture all strain-level variation or activity (no metatranscriptomics).
Related Publications
Explore these studies to deepen your understanding of the subject.