Medicine and Health
Specific intracellular signature of SARS-CoV-2 infection using confocal Raman microscopy
H. Salehi, A. Ramoji, et al.
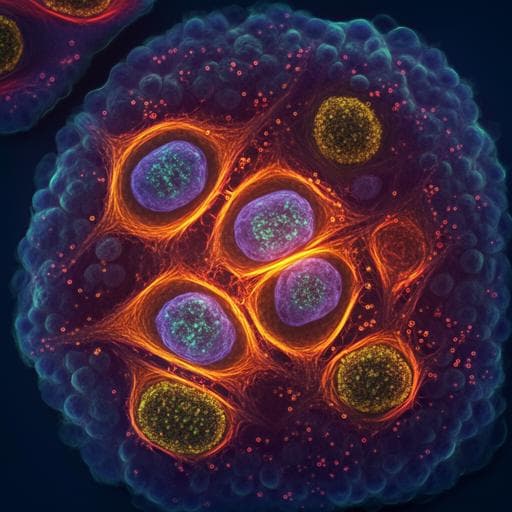
The study addresses how SARS-CoV-2 infection alters intracellular biochemistry and whether confocal Raman microscopy can provide a virus-specific molecular signature at the single-cell level. COVID-19 presents heterogeneous clinical profiles and a lack of reliable biomarkers for early detection and patient stratification. Conventional diagnostic methods (immunoassays, PCR, next-generation sequencing) are powerful but require prior knowledge of the pathogen, can be costly, and may be challenged by low viral loads. Raman microscopy offers label-free, noninvasive chemical profiling of single cells, enabling early detection of biochemical changes induced by viral infection without genetic/proteomic priors. The authors hypothesize that SARS-CoV-2 induces a distinct intracellular Raman signature, differentiable from another RNA virus (measles virus, MeV), and that multivariate analysis can classify infection status and virus type, potentially revealing biomarkers such as amino acid changes (e.g., tryptophan).
Prior work has established Raman spectroscopy and imaging as tools for chemical analysis of cells and tissues, enabling single-cell, label-free detection of biochemical changes. Unsupervised (e.g., PCA) and supervised (e.g., KMCA for organelle segmentation, SVM for classification) methods are standard for Raman data analysis. Viral detection using Raman approaches has been explored, including detection of RNA viruses in saliva and early detection of infection in live cells. SERS-based SARS-CoV-2 detection has shown high sensitivity but depends on engineered nanoparticle substrates, affecting cost and reproducibility. Recent studies reported Raman-based discrimination of cells infected with other viruses and used PCA/SERS to detect viral components. However, spontaneous (non-SERS) confocal Raman microscopy to interrogate SARS-CoV-2-induced intracellular biochemical changes and to compare them against another RNA virus at the organelle level has been less explored. This study builds on these advances to identify SARS-CoV-2-specific intracellular Raman signatures and classification models.
Cells and viruses: Vero E6 cells (African green monkey kidney; SIGMA #85020206) were cultured in DMEM with 10% heat-inactivated FBS at 37 °C, 5% CO₂. SARS-CoV-2 isolate BetaCoV/France/IDF0372/2020 (EVAg platform) was propagated in Vero E6 (DMEM + 2.5% FBS) and harvested 72 h post-inoculation. For experiments, Vero E6 cells on Raman glass slides were infected with 10^6 PFU SARS-CoV-2 (MOI 0.1) for 24 h; MeV (Schwartz strain) infection was performed similarly (MOI 0.1). Cells were fixed with 4% PFA at 24–48 h post-infection and washed prior to Raman imaging. All infection assays were performed in triplicate. Infection verification: SARS-CoV-2 infection in Vero E6 was confirmed by immunoblots (ACE2, Spike, N protein), immunofluorescence confocal microscopy (anti-M protein; 24 and 48 hpi), and transmission electron microscopy (viral particles at plasma membrane; intracellular DMVs/spherules near nucleus/mitochondria) at 24 hpi. Raman imaging: WITec Alpha 300 R confocal Raman microscope with 532 nm frequency-doubled Nd:YAG laser (50 mW), 60× Nikon water immersion objective (NA 1.0). Spatial resolution ~325 nm; axial ~991 nm; voxel ~300×300×900 nm. EMCCD detector captured scattered signals. CaF₂ substrates (characteristic 320 cm⁻¹ peak) minimized background. Central wavelength gating 610 nm; spectral ranges acquired included 400–1800 cm⁻¹ (fingerprint) and 2700–3050 cm⁻¹ (C–H stretching). Each scan contained >20,000 spectra; reconstructed images based on integrated C–H bands (2800–3100 cm⁻¹). Organelle segmentation: K-means cluster analysis (KMCA; WITec software) segmented spectra into clusters corresponding to cellular compartments (nucleus, nucleolus, mitochondria/Golgi, cytoplasm, lipid droplets). Mean spectra per organelle were extracted for downstream analysis. Preprocessing: For each biological replicate, 40 spectra/condition were extracted per intracellular component. Spectra truncated (360–3050 cm⁻¹), background subtracted using SNIP algorithm, further truncated to 400–1800 and 2700–3050 cm⁻¹, and vector normalized (R script). Difference spectra were generated (OriginPro) to visualize biochemical changes (control minus infected; MeV minus SARS-CoV-2). Savitzky–Golay smoothing (window 15, order 2) was used for display of difference spectra. Multivariate analysis: PCA performed separately on normalized spectra from nucleus, Golgi-mitochondria, and cytoplasm; 3D score plots and loadings examined to assess separation of groups. For classification, the first 13 PCs were used as inputs to SVM models (gamma=1e-4, cost=200, radial kernel, C-classification) with tenfold cross-validation. Two-class SVMs: (1) control vs MeV-infected; (2) control vs SARS-CoV-2-infected; (3) MeV vs SARS-CoV-2. A three-class SVM (control, MeV, SARS-CoV-2) was also built (Supplementary).
- SARS-CoV-2 and MeV infections produce distinct intracellular Raman signatures at 24 h post-infection, detectable in subcellular compartments (cytoplasm, Golgi–mitochondria, nucleus).
- Difference spectra (infected vs control) showed: prominent changes in C–H stretching region (2800–3050 cm⁻¹); phosphate backbone vibrations near 788–790 cm⁻¹ in cytoplasm and Golgi–mitochondria (consistent with viral RNA presence); lipid signatures (e.g., 1732 cm⁻¹; 2847/2864 cm⁻¹); nucleic acid ribose marker at 1125 cm⁻¹.
- SARS-CoV-2-infected cells displayed clear tryptophan vibrations (e.g., ~566–566/749 cm⁻¹; also 755, 1201, 1547, 1607 cm⁻¹ in loadings), whereas MeV-infected cells showed dominant protein bands (e.g., 2933/2970 cm⁻¹) and tyrosine signatures (815, 1629 cm⁻¹).
- PCA separated control from infected spectra across compartments; in the nucleus, SARS-CoV-2 and MeV spectra were well separated, indicating distinct nuclear biochemical profiles.
- SVM classification (tenfold cross-validated, PCs=13): • Control vs MeV: accuracy 98.89% (also reported as ~99%). • Control vs SARS-CoV-2: accuracy 97.22% (reported as ~97%). • MeV vs SARS-CoV-2: accuracy 97.78% (reported as ~98%).
- Spectral features distinguishing MeV vs SARS-CoV-2 included differences in protein bands (e.g., 1612 cm⁻¹ in SARS-CoV-2 vs 1656 cm⁻¹ in MeV), higher lipid signals in SARS-CoV-2 (2856, 2885 cm⁻¹), nucleic acids (1091, 1255 cm⁻¹ in MeV), and tryptophan at ~749 cm⁻¹ in SARS-CoV-2.
- TEM confirmed active SARS-CoV-2 replication and egress at 24 hpi (MOI 0.1), with viral particles at the plasma membrane and intracellular viral factories (DMVs/spherules).
- Genomic/proteomic analysis indicated SARS-CoV-2 proteome contains ~3× more tryptophan residues than MeV (159 vs 57 aa), supporting intracellular tryptophan accumulation observed by Raman.
- The observed intracellular tryptophan increase aligns with reported alterations of tryptophan/kynurenine in sera of COVID-19 patients, suggesting tryptophan as a potential biomarker.
The findings demonstrate that spontaneous confocal Raman microscopy, combined with KMCA, PCA, and SVM, can detect and classify virus-induced intracellular biochemical changes in Vero E6 cells. The robust separation of control vs infected cells and differentiation between SARS-CoV-2 and MeV across organelles, particularly in nuclear spectra, supports the premise that different RNA viruses induce distinct host-cell metabolic and molecular responses detectable by Raman signatures. The consistent presence of tryptophan bands in SARS-CoV-2-infected cells, contrasted with tyrosine prominence in MeV infection, suggests virus-specific amino acid/protein composition and metabolic alterations. The proteomic enrichment of tryptophan in SARS-CoV-2 provides a mechanistic rationale for the Raman-observed increase and links to clinical observations of altered tryptophan metabolism (kynurenine pathway) in COVID-19. High cross-validated SVM accuracies indicate that Raman spectral features can be leveraged both to detect infection and to discriminate virus type without labels or prior genomic information, underscoring the method’s potential for rapid, low-cost diagnostics and biomarker discovery. The approach may inform pathogenesis studies and therapeutic target identification by mapping organelle-specific biochemical perturbations during infection.
This work provides proof of concept that label-free confocal Raman microscopy can resolve virus-specific intracellular biochemical signatures and classify infection status and virus type with high accuracy. SARS-CoV-2 infection induces a distinctive Raman profile, notably increased tryptophan signals, differentiating it from measles virus in Vero E6 cells. The method integrates organelle-level spectral mapping (via KMCA) and multivariate analysis (PCA/SVM), offering rapid, non-destructive assessment of virus–host interactions. Future research should extend analyses to additional, clinically relevant human cell types and primary samples, validate tryptophan and other spectral markers as COVID-19 biomarkers, and explore translational implementations (e.g., Raman barcodes) for diagnostics and patient stratification.
- Experiments were performed on a single cell line (Vero E6) under in vitro, fixed-cell conditions; generalizability to other human cell types and in vivo/clinical samples remains to be validated.
- Although repeated in triplicate, biological and experimental heterogeneity required supervised methods (SVM) for robust classification; unsupervised PCA alone could not resolve pooled batches.
- Raman assignments infer biomolecular changes but do not provide direct molecular identification/quantification; complementary biochemical assays would strengthen interpretations.
- Time points were limited primarily to 24 h post-infection; temporal dynamics beyond this window were not extensively explored.
- The study compares only two RNA viruses; broader pathogen panels are needed to assess specificity across diverse infections.
Related Publications
Explore these studies to deepen your understanding of the subject.







