Medicine and Health
Skin-inspired, sensory robots for electronic implants
L. Zhang, S. Xing, et al.
This innovative research presents a new approach to soft robots that combine an electronic skin and artificial muscles, designed for versatile medical applications. Conducted by a team of experts including Lin Zhang and Sicheng Xing, these bio-inspired robots demonstrate remarkable functionalities like blood pressure detection and drug delivery, showcasing the tremendous potential in healthcare technologies.
~3 min • Beginner • English
Introduction
The study addresses the challenge of seamlessly integrating actuators, sensors, and controllers into soft, biocompatible robotic implants that can safely interact with dynamic biological environments. Inspired by the inseparable integration of sensory skin and skeletal muscles in vertebrates, the goal is to create soft, somatosensory robots that preserve physical softness, provide multimodal sensing, and enable adaptive, on-demand actuation for precision therapeutics. Prior soft-robotic implants demonstrate partial capabilities (e.g., capacitive bladder monitoring with shape-memory actuation for voiding; shape-memory polymer grippers measuring carotid pressure; hookworm-inspired thera-grippers for GI drug delivery) but face limitations in compliant mechanics, biocompatibility, structural adaptability, and biomimicry. The authors propose a bio-inspired, multilayer design composed of a multi-modal e-skin fabricated via an in situ solution-based approach and a thermally responsive hydrogel muscle to enable closed-loop sensing-actuation, wireless operation, and safe, stress-free interfacing with tissues and organs across multiple clinical scenarios.
Literature Review
The paper situates its contribution within soft implantable robotics and bioelectronics, referencing devices for bladder control, vascular sensing, gastrointestinal drug delivery, and cardiac assistance. Existing systems use shape-memory alloys/polymers, hydrogel actuators, and integrated sensors (capacitive, crack-based, etc.), but often lack seamless integration that maintains softness and biocompatibility, and they may be limited by fabrication methods (e.g., 3D printing, transfer processes) that hinder heterogeneity and multimodal integration. The authors highlight hydrogels (e.g., PNIPAM) for their softness, low activation temperature, and nonfibrotic biocompatibility, and emphasize opportunities to mimic biological receptors through heterogeneous nanocomposite e-skins (AgNWs, RGO, MXene, PEDOT:PSS in PI/PDMS). They identify unmet needs: compliant mechanics matching tissues, robust biocompatibility, structural reconfigurability, biomimicry for multi-functionality, and wireless, battery-free operation for minimally invasive deployment.
Methodology
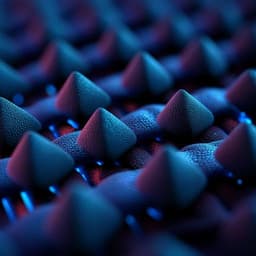
Design and materials: A bilayer soft robot comprising (i) an electronic-skin (e-skin) layer with multi-modal nanocomposites (AgNW/PI heater, RGO/PI thermal sensor, AgNW/PDMS strain sensor, PEDOT:PSS/PI electrodes; additional MXene sensors) fabricated via an in situ solution-based approach and parylene encapsulation (~2 μm), and (ii) an artificial muscle based on thermoresponsive PNIPAM hydrogel (LCST ~32–34 °C; ~90% volume reduction from 25–60 °C). A bio-adhesive (n-butyl cyanoacrylate) bonds layers.
Fabrication: Functional nanomaterial suspensions (AgNWs, RGO, PEDOT:PSS, MXene) are drop-cast/patterned on PI, followed by spin-casting liquid PI to infiltrate 3D networks and cure (150 °C, 1 h), embedding nanomaterials within PI. Laser cutting defines patterns. Parylene encapsulates e-skin; e-skin is bonded to PNIPAM. Variants include multi-layer stacking (e.g., PEDOT:PSS electrodes and RGO/PI sensor on opposite faces), starfish- and seedpod-inspired geometries, and a tri-layer pill (e-skin/muscle/e-skin) that self-expands in 3D.
Characterization: SEM, XPS, XRD, FTIR confirm nanocomposite integration and chemistry; IR thermography evaluates heaters under bending/twisting. Mechanical/adhesion tests include 180° peel and force output. Thermal/electrical sensing characterized for RGO/PI and MXene/PI thermal sensors (TCR, linearity, cycling), and AgNW/PI heater (power–temperature response, cycling). Finite Element Analysis (ABAQUS) predicts deformations (bending, twisting, expansion) and stress distributions.
Programmable actuation and sensing: Distributed AgNW/PI heaters enable local electrothermal actuation; embedded RGO/PI thermal sensors provide proprioceptive temperature feedback. Hydrogel thickness is tuned to balance deformation, force, and device compactness. Control algorithms on a microcontroller regulate heater current from temperature feedback to maintain setpoints and prevent overheating.
Wireless operation: Sensing uses a passive LC resonator with a PAAm hydrogel dielectric pressure sensor coupled inductively to a readout coil/VNA; actuation uses RF power harvesting via a receiving copper coil magnetically coupled to a transmitter, rectified to power heaters. A three-lead LC receiving network provides frequency-selective power delivery to individual heaters for multi-arm control. Effects of coil deformation (bending, twisting, distorting) on resonance and efficiency are measured and modeled.
Application demonstrations (in vitro/ex vivo/in vivo):
- Bladder gripper: PNIPAM actuator, 3D buckled strain sensor (serpentine Au/PI on elastic PAAm for conformal adhesion), BLE SoC for strain readout and PWM-driven electrotherapy; balloon model simulates filling/voiding for closed-loop stimulation at a volume threshold.
- Vascular cuff: PNIPAM muscle with e-skin strip pattern (45° to axis) forming a helix to encircle a tube with pulsatile flow; Au serpentine strain sensor measures pressure waveforms.
- Ingestible robot: Pill-sized tri-layer that expands in the stomach; PEDOT:PSS/PVA hydrogel pH sensor (pH 3–8), and PLGA-based drug patch (Rhodamine B model) for temperature-modulated release.
- Cardiac thera-gripper: Four-arm device with PNIPAM actuators, Au E-stim electrodes, two thermal sensors, and four Au/PI strain sensors; minimally invasive placement, actuation near body temperature; in vitro cytocompatibility (3T3-J-2) and in vivo mouse implantation, ECG/E-stim, echocardiography, and histology.
Biocompatibility and animal studies: 3T3-J-2 cells exposed to device materials and integrated devices at 37–39 °C for 48 h; histology after thoracic implantation in mice; in vivo cardiac function assessment including MI model (LCA ligation), ECG and echocardiographic FS/strain; device durability over 2 weeks.
Key Findings
- Materials integration and actuation: PNIPAM hydrogel exhibits ~90% volumetric shrinkage from 25–60 °C; LCST ~32–34 °C, tunable via AAm co-monomer. AgNW/PI heaters provide uniform heating under bending/twisting; LCST can be reached with <~1 W input power. Soft robotic finger generated up to ~32 mN static force at 40 °C with stable output over 40 on/off cycles; thicker hydrogel increases deformation and force but slows response and increases device volume.
- Thermal sensing: RGO/PI thermal sensor shows linear resistive response with TCR >0.5%/°C, conductivity ~400 S/m, stable after 1000 bending cycles and PBS immersion; cycling reproducibility and accuracy comparable to a commercial thermal resistor (ERT-J0ET102H). MXene/PI thermal sensors also show linear temperature response (23–55 °C). Embedded sensors enable proprioceptive temperature mapping of local regions.
- Programmable morphing: Localized heaters and sensors enable stepwise coiling and independent control of multi-arm grippers; geometry (parallel strips) produces twisting/helix modes; pill design expands into a 3D ring in response to heating.
- Wireless systems: Passive LC pressure sensor (PAAm dielectric) shows linear ΔC/C0 vs pressure (0–3.5 kPa) with gauge factor ~−3%/kPa; resonant frequency shifts from ~340 to ~260 MHz across the pressure range with sensitivity ~−26.7 kHz/kPa. RF power harvesting peaks at ~15 MHz with harvested power ~1.05 W and ~80% efficiency, sufficient to actuate heaters; IR shows localized heater warming with minimal coil heating. Coil deformation alters coupling efficiency but maintains resonant frequency and sufficient power for actuation.
- Bladder model: 3D buckled strain sensor adheres conformally; resistance correlates linearly with balloon volume during fill/void cycles; closed-loop control initiates electrical stimulation at a set threshold (e.g., 100 mL) and deactivates post-voiding, demonstrating wireless closed-loop sensing-therapy.
- Vascular cuff model: Helical cuff achieves gentle enclosure; strain sensor output linearly correlates with internal fluid pressure and captures pulsation waveforms continuously.
- Ingestible platform: Device expands in stomach model to prevent pyloric passage; PEDOT:PSS/PVA pH sensor shows linear response from pH 3–8; PLGA/RhB patch releases drug with temperature-dependent kinetics over 1 h.
- Cardiac thera-gripper in vivo: Device grasps mouse epicardium with minimal disruption; temperature sensors monitor deployment thermal changes; Au E-stim electrodes deliver impulses (0.5–2 V, 1 ms, ~2.65 Hz) with ECG confirmation; multi-strain sensors record chamber-specific contractions and cardiac cycles in real-time. In MI model, echocardiographic fractional shortening decreased from ~75% to ~15%; thera-gripper strain sensors detected reduced RV/LV strain and heart rate consistent with infarction. Cytocompatibility maintained (3T3-J-2) at 37–39 °C; histology showed no observable inflammation; device function (E-stim and thermal sensing) remained stable over 2 weeks.
Discussion
The integrated e-skin and hydrogel-muscle architecture emulates biological skin-muscle synergy, enabling closed-loop sensing-actuation with mechanical compliance matched to tissues. The in situ nanocomposite approach achieves thin, flexible e-skins with heterogeneous, multimodal sensors and stimulators, overcoming interfacial resistance and dispersion challenges of conventional composites and offering compact, high-performance modules. Electrothermal actuation provides precise, regional morphing controlled by embedded temperature feedback, achieving safe and adaptable motion in confined biological spaces. Wireless, battery-free LC sensing and RF power harvesting reduce implant size and complexity and enable selective activation of distinct actuators via frequency multiplexing. Application-specific prototypes demonstrate safe, conformal interfacing and functional relevance: continuous bladder volumetry with closed-loop stimulation, vascular pressure monitoring via a self-forming helix cuff, a gastric-resident platform for pH sensing and drug release, and a thera-gripper for epicardial sensing and electrotherapy that quantifies regional myocardial mechanics and operates in vivo. These results directly address the research goal of creating minimally invasive, intelligent implants that adapt structurally while providing multimodal sensing and therapeutic functions, highlighting translational potential across multiple organ systems.
Conclusion
This work introduces a universal, bio-inspired strategy for soft implantable robots that coherently integrate an in situ-fabricated multimodal e-skin with a thermoresponsive hydrogel muscle to achieve adaptive, wireless, closed-loop sensing and actuation. The platform supports diverse geometries and motions (bending, twisting, expanding), integrates varied sensing/stimulation modalities (temperature, strain, pressure, pH, electrical/thermal stimulation), and maintains biocompatibility and conformal interfacing. Demonstrations across bladder control, vascular monitoring, gastric pH sensing/drug delivery, and epicardial sensing/electrotherapy, including in vivo validation in a mouse model, establish feasibility for next-generation medical implants with structural intelligence. Future work should focus on chronic stability and encapsulation in dynamic physiological environments, long-term biocompatibility and fibrosis prevention, optimization of wireless power and communication in deep tissues, energy-efficient control algorithms, and patient-specific design customization for personalized therapies.
Limitations
- Many demonstrations are in vitro or ex vivo; comprehensive chronic in vivo evaluations across all device types are pending.
- Electrical stimulation parameters for bladder control were not optimized; efficacy varies between individuals and requires further clinical investigation.
- Hydrogel-based adhesion strength decreases near LCST and with dehydration; long-term fixation may require supplementary anchoring strategies.
- Increasing hydrogel thickness enhances force but reduces compactness and response speed, impacting minimally invasive deployment.
- Hydrogel pressure sensors can swell; the paper proposes encapsulation and increased crosslinking to mitigate, but long-term stability in vivo remains to be validated.
- Wireless power transfer efficiency decreases with coil misalignment and deformation; although sufficient for actuation here, robustness in varied anatomical positions requires further optimization.
- Potential thermal risks from electrothermal actuation are mitigated by feedback control but need thorough safety margins for clinical translation.
Related Publications
Explore these studies to deepen your understanding of the subject.