Medicine and Health
Rapid 3D imaging at cellular resolution for digital cytopathology with a multi-camera array scanner (MCAS)
K. Kim, A. Chaware, et al.
The study addresses the challenge of rapidly digitizing thick cytopathology smears, which require high-resolution, large field-of-view, and 3D imaging. Conventional whole slide imaging (WSI) systems are slow, expensive, and limited in 3D capture, often taking over an hour per slide for thick smears. Cytology smears span large lateral areas (up to 75 x 25 mm) and depths (>50 µm), with cellular features at ~1 µm scale, creating a fundamental trade-off between field-of-view and resolution in single-objective microscopes. Rapid on-site evaluation (ROSE) is time-critical but resource-intensive. The research question is whether a parallelized multi-camera microscope can overcome etendue limits to rapidly scan thick smears in 3D across entire slides at cellular resolution, enabling remote viewing and machine learning-assisted analysis to improve clinical workflows and diagnostic efficiency.
Background includes the fundamental FOV–resolution trade-off and etendue limits in single-lens microscopes. Standard WSI enables digitization and software analysis but is optimized for thin sections and is slow/less practical for thick smears. Alternative computational imaging methods (Structured Illumination Microscopy and Fourier Ptychography) increase resolution with large-FOV optics but require multiple sequential illuminations and computational reconstructions, limiting speed and still providing smaller FOVs than whole slides, especially for thick specimens. Multi-aperture/array imaging systems have been used for macroscopic imaging, light-field capture, and compact designs. Prior multi-camera array microscope (MCAM) work achieved large-area imaging (≥100 cm²) at 5–20 µm resolution for model organisms but lacked sufficient axial scanning and cellular resolution necessary for cytology. The scarcity of fast WSI for thick smears has also limited the development of automated analysis software for cytopathology.
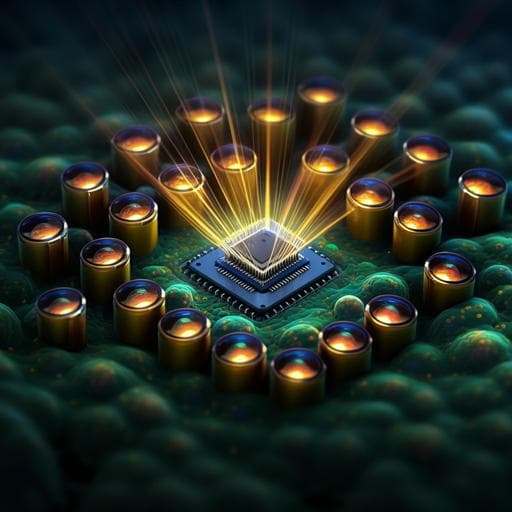
Hardware and optics: The Multi-Camera Array Scanner (MCAS) integrates 48 identical modules in a 6 x 8 grid with 9 mm pitch on a single PCB. Each module uses a 13 MP CMOS sensor (Onsemi AR1335, 4208 x 3120, 1.1 µm pixels) and a custom finite-conjugate objective. Two lens designs were used: (i) Edmund Optics: 2.2x magnification, NA 0.3, WD 3.05 mm (≈10x equivalent), achieving 1.2 µm full-pitch resolution; (ii) Avantier Inc.: 6.89x, NA 0.5, WD 1.74 mm (≈20x equivalent), achieving 0.6 µm full-pitch resolution. The array targets a 54 x 72 mm² scan area accommodating three slides. Motion and acquisition: Samples move via three motorized stages (Zaber) for lateral and axial scanning. Due to the 9 mm inter-camera pitch, lateral scans cover only up to 9 x 9 mm² rather than the full slide length. For NA 0.3, a 7 x 7 lateral grid (≈1.3 mm steps) per axial plane is used; for NA 0.5, a 20 x 20 grid (≈0.46 mm steps). Axial stacks cover 120–150 µm with step sizes of 5 µm (NA 0.3) or 1 µm (NA 0.5). All 48 cameras capture synchronously (≤6 µs offset). Per snapshot: ~0.63 gigapixels raw (48 x 4208 x 3120); center-cropped to 3072 x 3072 per camera for optimized transfer yielding ~0.45 GP per snapshot. Data streamed via FPGA at up to ~5 GP/s (≈5 GB/s), enabling up to 8 fps; exposure 50 ms with on-the-fly saving during axial motion (scan speeds ~34 µm/s for NA 0.3, ~7 µm/s for NA 0.5). Per-plane composites: 16 GP (NA 0.3, 2352 FOVs) or 140 GP (NA 0.5, 19,200 FOVs). Illumination uses a 16 x 24 RGB LED array (9 mm pitch) beneath a diffuser. Preprocessing and stitching: For each lateral position, the most in-focus z-plane is selected via a Laplacian contrast metric (7 x 7 kernel). Adjacent planes around the in-focus plane are also kept for refocusing during review. White balance via per-channel histogram matching to clinical references and flat-field correction are applied. Stitching uses the Hugin open-source framework with global transformations (shift/rotation/scale), bootstrapped by parameters from a printed calibration target to handle sparse-feature regions. Stitching of 49 images per camera takes <1 min plus ~9–10 min for intensity correction; operations are parallelizable across cameras. Visualization: Gigaviewer (OpenSeadragon-based) supports pan/zoom with multiresolution tiles and axial refocusing across planes for remote 3D review of 16 GP composites; example images hosted at https://gigazoom.rc.duke.edu. Specimens and experiments: Rapid whole-slide 3D imaging was demonstrated on 16 Diff-Quik–stained lung FNA samples (axial range ~120 µm). With NA 0.3 and 5 µm steps, three slides (54 x 72 mm² total area) were imaged in <5 min (<2 min/slide). With NA 0.5 and 1 µm steps, acquisition took ~40 min for the same volume due to denser lateral sampling and smaller DOF. Adequacy assessment (ROSE) on thyroid FNAs: 26 Diff-Quik–stained thyroid FNA smears were labeled adequate/inadequate by one pathologist via conventional microscopy (ground truth: 18 adequate, 8 inadequate). Three pathologists independently reviewed MCAS digitizations via Gigaviewer; majority vote used for predicted labels. Object detection for adenocarcinoma localization: Five lung FNA smears (adenocarcinoma-positive and benign) imaged with NA 0.3. For ML, per-sensor images (3072 x 3072) were split into four 1536 x 1536 patches. Clinicians annotated suspected adenocarcinoma regions with bounding boxes. Total patches: 1794 (train/val/test = 1201/384/209), with patches from a given sensor image kept within a single split. YOLOv7 was trained for detection; performance reported with mAP and recall. Slide-level classification via Multiple Instance Learning (MIL): 16 labeled lung FNA slides (8 positive adenocarcinoma, 8 negative). From each sensor image, nine 1024 x 1024 sub-patches formed instances; eight bags per slide were created (128 bags total). Assumption: positive slide implies at least one positive instance per bag; negative slide implies all-negative instances. Four-fold cross-validation was conducted at the slide level (groups of 4 slides, 2 positive/2 negative), with all bags from a slide confined to a single fold. Bag-level metrics and slide-level majority voting were computed.
- Speed and scale: MCAS captures 624 MP per synchronized snapshot and streams up to ~5 GP/s, enabling rapid 3D imaging. With NA 0.3 (7 x 7 lateral scans; 5 µm axial steps), three slides over 54 x 72 mm² were digitized in <5 minutes total (<2 minutes/slide). With NA 0.5 (20 x 20; 1 µm steps), acquisition took ~40 minutes. Each focal plane composite is ~16 GP (NA 0.3) or ~140 GP (NA 0.5).
- Resolution: Achieved 1.2 µm full-pitch resolution with NA 0.3 optics and 0.6 µm with NA 0.5, supporting cellular/subcellular visualization.
- Adequacy assessment (thyroid ROSE): On 26 smears, MCAS-based remote adequacy assessment (majority of three pathologists) achieved sensitivity 100% and specificity 94.4% vs. conventional microscopy ground truth (18 adequate, 8 inadequate).
- Adenocarcinoma localization (lung FNAs): YOLOv7 achieved mean average precision (mAP) 0.645 and recall 0.73 for detecting suspected adenocarcinoma regions across 1794 patches.
- Slide-level adenocarcinoma classification (lung FNAs, MIL): Four-fold cross-validation yielded mean bag-level accuracy 0.930, precision 0.931, recall 0.938, and AUC 0.969; slide-level accuracy 100% via majority vote across all folds.
- Workflow enablement: Custom Gigaviewer enabled remote, interactive 3D review with axial refocusing of 16 GP composites, supporting potential clinical telecytology and ROSE workflows.
The MCAS overcomes traditional etendue limitations by parallelizing image capture with 48 synchronized micro-cameras, enabling orders-of-magnitude faster 3D digitization of thick cytology smears than conventional WSI at similar component cost. It supports remote whole-slide 3D review via Gigaviewer and integrates machine learning to triage regions of interest and perform slide-level classification. The adequacy assessment results indicate parity with current ROSE practice while enabling remote, rapid decisions. Object detection demonstrates feasibility for highlighting suspicious regions to expedite pathologist review, prioritizing recall to minimize false negatives under sparse/inconsistent annotations. MIL-based slide-level classification achieves high accuracy and AUC even with limited slides, showing promise for rapid diagnostic screening without exhaustive cell-level labels. To further accelerate acquisition, reducing lateral overlap (e.g., 6 x 6 scans instead of 7 x 7) and increasing axial step size could cut total acquisition time by an estimated 63% while still supporting ML workflows that tolerate modest defocus. Future improvements include learned/programmable illumination to enhance discriminative features, leveraging full 3D stacks (beyond all-in-focus images) for ML, and adding fluorescence to expand diagnostic capabilities and enable high-throughput generation of multimodal image pairs. Early stopping of scanning upon ML-detected positives could further shorten time to diagnosis.
This work introduces the Multi-Camera Array Scanner (MCAS), a 48-camera parallelized microscope that rapidly digitizes thick cytology smears across three slides at cellular resolution, producing multi-gigapixel 3D datasets suitable for remote review. The system achieves submicron resolution (0.6–1.2 µm), captures up to 5 GP/s, and scans three slides in minutes (NA 0.3), substantially outperforming conventional WSI for thick smears. Integrated ML pipelines demonstrate feasibility for suspected adenocarcinoma localization and high-accuracy slide-level classification, and MCAS-enabled remote adequacy assessment matches standard ROSE performance. The contributions collectively enable new digital cytopathology workflows, including telecytology and rapid on-site evaluation. Future work will focus on accelerating acquisition by optimizing scan patterns and axial steps, exploiting 3D information and learned illumination, incorporating fluorescence imaging, and validating ML models on larger, multi-institutional datasets.
- Acquisition-time trade-offs: Higher-resolution NA 0.5 imaging requires finer axial steps (1 µm) and denser lateral scans (20 x 20), increasing total acquisition (~40 min) versus NA 0.3 (~5 min).
- Data throughput bottleneck: Current FPGA pipeline limits streaming to ~5 GP/s, constraining further speed gains without architecture upgrades.
- Optical aberrations: Resolution degrades toward FOV edges and field curvature varies per lens; corrections are partial via focal stacking and potential FOV cropping for visualization.
- Algorithmic focus detection: Laplacian-based focus metrics can fail in low-texture regions or with sensor/cover-slip artifacts, causing occasional focus plane misidentification.
- ML dataset size and labeling: Object detection used only five slides and 1794 patches with sparse/inconsistent annotations, limiting precision and generalizability. Slide-level MIL used 16 slides, necessitating cross-validation and assumptions (e.g., positive slides contain positive instances in each bag). Larger, diverse, multi-annotator datasets are needed.
- Generalizability and clinical validation: Results are based on archival Diff-Quik–stained thyroid and lung FNAs from a single center; broader multi-site validation and inclusion of additional stains and cancer types are required.
- Hardware complexity and cost: Although component costs target parity or reduction versus WSI, multi-camera alignment, calibration, and maintenance add system complexity.
Related Publications
Explore these studies to deepen your understanding of the subject.