Medicine and Health
Radiogenomics for predicting p53 status, PD-L1 expression, and prognosis with machine learning in pancreatic cancer
Y. Iwatate, I. Hoshino, et al.
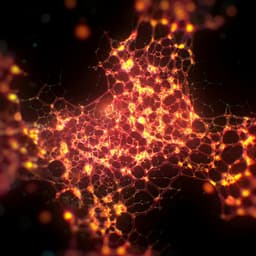
This groundbreaking study delves into the realm of radiogenomics, spotlighting its potential to predict p53 mutations and PD-L1 expression in pancreatic ductal adenocarcinoma (PDAC). With significant findings linking p53 mutations to poor prognosis, this research led by Yosuke Iwatate and collaborators opens new doors for precision medicine in PDAC treatment.
Related Publications
Explore these studies to deepen your understanding of the subject.