Medicine and Health
PSCA-CAR T cell therapy in metastatic castration-resistant prostate cancer: a phase 1 trial
T. B. Dorff, M. S. Blanchard, et al.
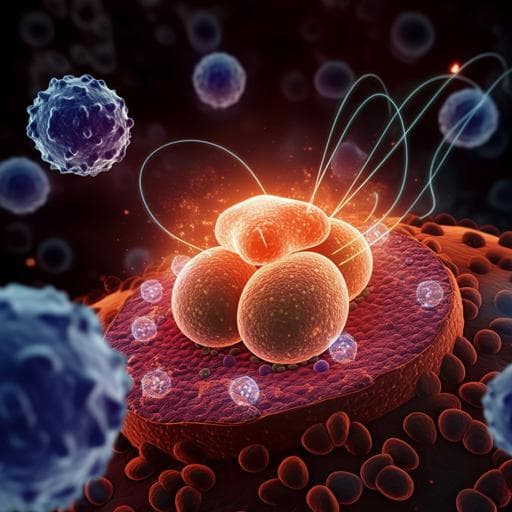
Metastatic castration-resistant prostate cancer (mCRPC) is a lethal disease with over 30,000 annual deaths in the United States. Prior immunotherapies, including vaccines (GVAX, Prost-VAC) and checkpoint inhibitors (CTLA-4, PD-1), have shown limited activity in mCRPC; sipuleucel-T is the only approach shown to prolong survival, underscoring the need for more effective strategies. Prostate tumors, particularly in advanced stages, are characterized by immunosuppression that limits T cell trafficking and effector function within the tumor microenvironment. However, tumor-associated antigens such as prostate stem cell antigen (PSCA) and prostate-specific membrane antigen (PSMA) are commonly and robustly expressed and represent promising targets for cellular immunotherapy. Building on preclinical studies demonstrating safety and efficacy of PSCA-directed CAR T cells with 4-1BB co-stimulation in prostate cancer models, this first-in-human phase 1 study aimed to evaluate the safety, tolerability, expansion/persistence, and preliminary antitumor activity of PSCA-CAR T cells in patients with mCRPC.
The paper situates the work within the broader immunotherapy landscape for mCRPC, noting the limited efficacy of prior vaccine-based strategies (GVAX, Prost-VAC) and immune checkpoint inhibitors (CTLA-4, PD-1). Sipuleucel-T, while offering a survival benefit, has modest impact, highlighting the gap for effective immunotherapies. Preclinical evidence supports PSCA as a target due to its high expression in prostate cancer and increased expression in advanced disease, especially bone metastases. Prior preclinical data with second-generation PSCA-CAR T cells employing 4-1BB co-stimulation showed safety and efficacy in eradicating bone metastatic disease in models, providing rationale for clinical translation of PSCA-directed CAR T therapy.
Design: Single-center, first-in-human, phase 1 dose-escalation trial at City of Hope (NCT03873805) evaluating safety and bioactivity of PSCA-directed, lentivirally transduced CAR T cells in men with mCRPC. Cohorts and dosing: Three dose levels (DLs) evaluated 100 million (M) CAR T cells with varying lymphodepletion (LD): DL1, 100 M without LD; DL2, 100 M with fludarabine/cyclophosphamide (Flu/Cy) LD (cyclophosphamide 500 mg/m2 i.v. days −5 to −3; fludarabine 30 mg/m2 i.v. days −5 to −3); DL3, 100 M with reduced cyclophosphamide LD (300 mg/m2 days −5 to −3) and the same fludarabine schedule. G-CSF was not given prophylactically but allowed for neutropenia. Endpoints: Primary endpoints were safety and dose-limiting toxicities (DLTs). Secondary endpoints included CAR T expansion and persistence to 28 days post-infusion (by flow cytometry and WPRE qPCR), PSA decline and RECIST response, and 6-month survival. Exploratory endpoints assessed immune cell phenotypes in blood, tumor-infiltrating lymphocytes, and serum cytokines. Additional planned exploratory endpoints (CTC RNA-seq, cfDNA WES, anti-CAR antibodies) were not reported in this paper. Eligibility: Men with mCRPC with progression after at least one androgen receptor pathway inhibitor (abiraterone or enzalutamide); prior taxane allowed but not required. Key labs: creatinine clearance ≥50 ml/min, AST/ALT ≤5 × ULN, bilirubin ≤2.0 mg/dl; LVEF ≥40%; no significant arrhythmia or CNS disease; no HIV or active HBV/HCV or uncontrolled infection. PSCA expression by IHC was required on archival or on-study tissue (≥30% tumor cells; moderate or higher staining). On-study biopsy and confirmation of PSCA staining were required for soft-tissue metastases; bone metastases confirmation was not required due to IHC assay calibration limitations. Trial conduct: Participants underwent consent, PSCA screening, leukapheresis, and product manufacturing. Imaging (CT and bone scan) and biopsies were obtained pre- and approximately day 28–30 post-infusion. Patients were hospitalized for infusion and at least 7 days follow-up; required to remain within 40 minutes of the center for the first 28 days. Toxicities were graded per CTCAE v4; DLTs were grade ≥3 (grade ≥4 hematologic) toxicities attributable to CAR T within 28 days, with standard CAR T exceptions; detailed organ-specific criteria applied. Design specifics: Dose escalation and cohort decisions followed the Toxicity Equivalence Range design (TEQR) with an equivalence range of 0.20–0.35 and too-toxic level 0.51. Initial participants at DL1 and DL2 were staggered through the DLT window. Planned escalation beyond 100 M was contingent on tolerability; protocol was amended after observing cystitis DLTs to reduce cyclophosphamide dose (DL3). Bridging therapy was permitted at physician discretion. Manufacturing: Autologous PBMCs were CD14+ and CD25+ depleted, stimulated with CD3/CD28 Dynabeads, and transduced with a PSCA(dCH2)BBZ/CD19t lentiviral vector (MOI 0.3), then expanded 12–17 days with IL-2 and IL-15. The CAR used a humanized anti-PSCA scFv, ACH2 spacer, CD4 transmembrane, 4-1BB co-stimulatory, and CD3ζ signaling domains; CD19t was used as a transduction marker. Released products showed a median 86.8% CAR positivity and a dominant central memory phenotype; two products were infused with FDA permission despite WPRE copy number outside prespecified limits. Median time from leukapheresis to infusion was 73 days (range 34–182). Six patients received bridging therapy (cabazitaxel n=4; cabazitaxel+carboplatin n=1; enzalutamide n=1). Assessments: PSA every ≥2 weeks during the DLT window, then day 60 and 90. CT and bone scans at baseline and days 28–30, then day 90 and q12 weeks. Peripheral blood immune monitoring included flow cytometry for CAR T identification (CD3+CD19t+) and phenotype markers (e.g., PD-1, CD25, CD95), WPRE qPCR for CAR T quantification, multiplex serum cytokines (Luminex), and in selected patients single-cell RNA-seq and TCR-seq of T cells (10x Genomics). CTCs were quantified via high-definition single-cell analysis (HDSCA). Tumor biopsies underwent IHC and multispectral immunofluorescence for immune and tumor markers.
- Accrual and cohorts: 58 screened for PSCA by IHC; 22 underwent leukapheresis; 14 infused (Aug 2019–Jul 2022). Cohorts: DL1 (100 M without LD, n=3), DL2 (Flu/Cy LD + 100 M, n=6), DL3 (reduced cyclophosphamide LD + 100 M, n=5).
- Safety and DLTs: No DLTs in DL1. DL2 had two DLTs of noninfectious cystitis (grade 3), prompting protocol amendment to DL3 with reduced cyclophosphamide dose and enhanced monitoring; DL3 had no DLTs and maximum cystitis grade 2.
- CRS and hematologic toxicity: CRS occurred in 5/14 (36%) with maximum grade 2; median onset 4 days (range 3–8). Tocilizumab was given to 3 patients; no grade ≥3 CRS, hypotension, hypoxia, high-grade neurotoxicity, or MAS/HLH. Grade ≥3 neutropenia: 0/3 (0%) DL1, 6/6 (100%) DL2, 3/5 (60%) DL3.
- Efficacy signals: PSA declines from baseline to day 28 occurred in 1/3 (DL1), 3/6 (DL2), and 3/5 (DL3). Overall, 4/14 (29%) had PSA declines >30% within 28 days; only one maintained >30% decline beyond day 28. RECIST best response stable disease: 0% (DL1), 67% (4/6) in DL2, and 60% (3/5) in DL3. Six-month survival: 33% (DL1), 67% (DL2), 40% (DL3). Radiographic improvements were observed in select patients, including liver lesion reduction in DL3 and soft tissue improvements in a DL2 responder.
- Representative responder (DL2): One patient (UPN388) had >90% PSA decline (64.2 to 3.5 ng/mL by day 28) with radiographic soft tissue improvement (RECIST stable disease due to bone lesions). This patient exhibited transient cytokine induction (e.g., IFNγ, IL-6, GM-CSF, IP-10, MIG) and dynamic immune changes including expansion of CD8+ central/effector memory subsets, increased PD-1 expression on CAR and non-CAR T cells, elevated CX3CR1 expression, increased effector CD8+ subsets (by scRNA-seq), and transient TCR clonal expansions.
- CAR T kinetics: CAR T expansion in peripheral blood was greater with LD (DL2/DL3) than without (DL1) by flow cytometry and WPRE qPCR. Reduced LD in DL3 showed similar expansion compared to DL2 in this small cohort. Overall CAR T persistence beyond 28 days was limited.
- CTCs: CK+ CTCs were detected in 100% of treated patients. Marked declines in mean CK+ cells from baseline to 28 days were seen in LD cohorts (DL2 and DL3), but not in DL1.
- Genomics: Among 8 patients with somatic testing, tumor mutational burden was low except one at 10.5. PTEN loss in three patients included the one with the greatest PSA decline. A DL3 patient with radiographic improvement in liver metastases had a CDK12 alteration and had progressed on prior checkpoint inhibitor therapy.
The trial demonstrates that PSCA-directed CAR T cells can be safely administered to patients with mCRPC and can induce biochemical (PSA declines) and radiographic improvements, particularly when preceded by lymphodepletion. The principal DLT was cystitis, consistent with an on-target/off-tumor effect potentially exacerbated by cyclophosphamide. Reducing cyclophosphamide from 500 to 300 mg/m2 decreased high-grade cystitis without clear loss of CAR T expansion in blood, suggesting that optimizing LD can improve the therapeutic index in solid tumor CAR T therapy. LD enhanced CAR T expansion and serum cytokine induction and was associated with higher rates of disease stabilization and CTC reduction, aligning with preclinical data showing improved intratumoral T cell infiltration and reduced myeloid suppression after cyclophosphamide. Despite on-treatment expansion and signs of immune activation (including endogenous TCR repertoire dynamics), limited CAR T persistence beyond 28 days likely contributed to the lack of durable remissions. Compared with other mCRPC CAR T studies, this PSCA-targeting approach showed a favorable safety profile with no high-grade neurotoxicity or MAS/HLH. Collectively, the findings validate PSCA as a therapeutic target and support further clinical development focusing on LD optimization, strategies to prolong CAR T persistence, and rational combinations to enhance durability and depth of response.
This first-in-human phase 1 study of PSCA-CAR T cells in mCRPC establishes safety at 100 M cells with and without LD and identifies noninfectious cystitis as the DLT at standard-dose cyclophosphamide LD. Reduced-dose cyclophosphamide mitigated high-grade cystitis while maintaining CAR T expansion in peripheral blood. Evidence of antitumor activity included PSA declines, radiographic improvements, and CTC reductions, particularly in LD cohorts, though CAR T persistence beyond 28 days was limited and durable remissions were not achieved. These results validate PSCA as a viable CAR T target in prostate cancer and motivate phase 1b/2 studies to optimize LD regimens, enhance CAR T persistence (e.g., cellular phenotype enrichment, manufacturing interventions), and test combinatorial strategies (chemotherapeutic or immunomodulatory) to improve durability and clinical benefit. Outpatient administration with close monitoring appears feasible given the favorable toxicity profile.
Key limitations include the small sample size inherent to a phase 1 trial, single-center design, and accrual challenges related to tissue pre-screening requirements, manufacturing and protocol holds, and potential selection bias against patients with rapidly progressive disease or marginal performance status. The lack of a validated PSCA IHC cutoff and variable assay calibration for bone biopsies may have affected patient selection. Limited CAR T persistence beyond 28 days constrained durable responses. The study was not powered to compare LD regimens definitively or to correlate genomic features with response. Some planned exploratory analyses (CTC RNA-seq, cfDNA, anti-CAR immunogenicity) were not reported here.
Related Publications
Explore these studies to deepen your understanding of the subject.