Medicine and Health
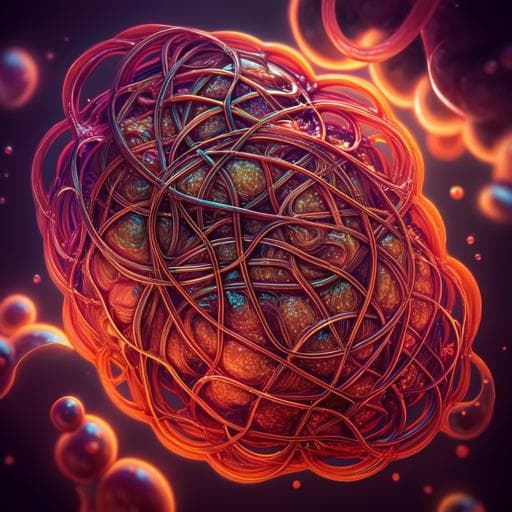
Progression of Cystic Fibrosis Lung Disease from Childhood to Adulthood: Neutrophils, Neutrophil Extracellular Trap (NET) Formation, and NET Degradation
M. A. Khan, Z. S. Ali, et al.
This groundbreaking research by Meraj A. Khan, Zubair Sabz Ali, Neil Sweezey, Hartmut Grasemann, and Nades Palaniyar delves into the complex interplay of neutrophils and NETs in cystic fibrosis, revealing how inflammation and infection lead to devastating lung damage. Discover the potential for new therapies that enhance the beneficial effects of neutrophils while mitigating the harmful impacts of NETs.
Related Publications
Explore these studies to deepen your understanding of the subject.