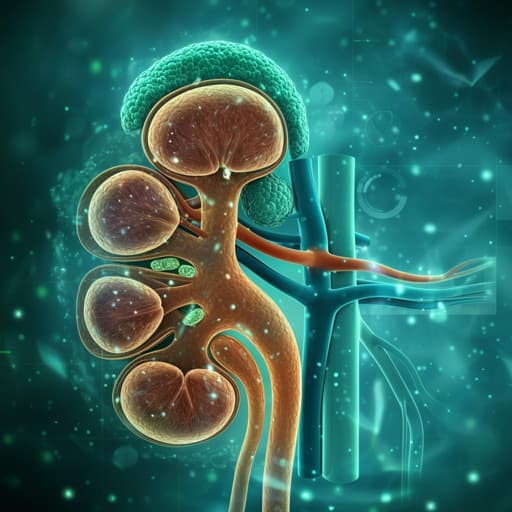
Medicine and Health
Novel Biomarkers for Early Detection of Acute Kidney Injury and Prediction of Long-Term Kidney Function Decline after Partial Nephrectomy
M. Allinovi, F. Sessa, et al.
This groundbreaking research by Marco Allinovi and colleagues uncovers promising noninvasive biomarkers, NephroCheck and kineticGFR, that can predict acute kidney injury (AKI) and potential long-term kidney function decline post robotic Nephron-Spearing Surgery. The early identification of these risks as early as 10 hours after surgery could revolutionize postoperative care.
Related Publications
Explore these studies to deepen your understanding of the subject.