Medicine and Health
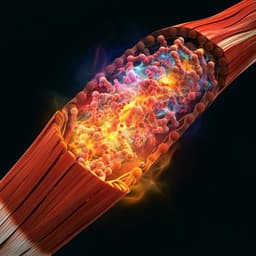
Neural cell integration into 3D bioprinted skeletal muscle constructs accelerates restoration of muscle function
J. H. Kim, I. Kim, et al.
Discover how the integration of neural cells into bioprinted skeletal muscle constructs, researched by Ji Hyun Kim and colleagues, can significantly enhance muscle regeneration. This innovative approach not only promotes myofiber formation and NMJ development but also restores muscle weight and function in vivo, paving the way for advanced therapies for muscle injuries.
~3 min • Beginner • English
Introduction
Extensive skeletal muscle defect injuries (>20% mass loss) result in irreversible functional impairment and are poorly addressed by current reconstructive options due to limited graft availability and donor-site morbidity. Tissue-engineered skeletal muscle constructs with aligned myofibers can recapitulate native structure, but delayed innervation in vivo limits full functional recovery. The study asks whether integrating human neural stem cells (hNSCs) with human muscle progenitor cells (hMPCs) in 3D bioprinted constructs can promote myofiber maturation, pre-form neuromuscular junctions (NMJs), accelerate host innervation, and improve functional restoration after volumetric muscle loss. The hypothesis is that neural-muscle cellular crosstalk and pre-formed NMJs enhance muscle survival, differentiation, and rapid integration with host nerves, leading to faster recovery of muscle mass and force.
Literature Review
Prior work has induced myofiber alignment via mechanical and electrical stimulation or micro-patterned scaffolds, improving in vitro maturation with some in vivo promise. Co-culture with endothelial cells and fibroblasts enhances vascularization and survival; 3D human muscle models with endothelium have been used to study fibrosis. Neuron–muscle co-cultures elucidate NMJ development, and 3D bioprinting enables precise spatial organization of multiple cell types and biomaterials to mimic native tissue. The authors' previous bioprinted human skeletal muscle constructs formed aligned myofiber bundles and improved structure and function in rodents, but complete restoration at 8 weeks was limited, likely due to delayed innervation. While skeletal muscle depends on NMJs for survival and function and denervation leads to atrophy, few studies have demonstrated in vivo innervation and functional improvements of engineered constructs. Neurotrophic factors and neurotransmitters from neural components can enhance myogenesis and NMJ maturation, suggesting neural integration may overcome the innervation bottleneck.
Methodology
Study design: Optimize hMPC:hNSC ratios in 2D co-culture, then fabricate 3D bioprinted skeletal muscle constructs at the optimal ratio for in vitro assessment and in vivo implantation into a rat tibialis anterior (TA) volumetric muscle loss model. Outcomes include cell viability, myogenesis, NMJ formation/function in vitro, and muscle mass, force, histology, innervation, and vascularization in vivo.
Cells: hMPCs isolated from de-identified human gracilis muscle biopsies under IRB approval, expanded to passages 1–4 in DMEM-based growth media with FBS and chicken embryo extract. hNSCs (ReNcell VM) expanded to passages 4–6 in maintenance medium with EGF and bFGF.
2D co-culture optimization: hMPCs and hNSCs plated on laminin-coated chambers across ratios 1:0 to 500:1 (constant hMPC number), differentiated up to 10 days. Differentiation media used DMEM/high glucose with 2% horse serum, ITS, dexamethasone, and antibiotics; hNSC differentiation used maintenance medium without growth factors. Assays included immunofluorescence for MHC, MyoD, myogenin; neural markers GFAP, βIII-tubulin (βIIIT), neurofilament (NF); AChR clustering; and NMJ colocalization (βIIIT/NF with AChR on MHC+ myotubes). Quantified myotube length, diameter, nuclei per myotube, striation, AChR density, and NMJ counts.
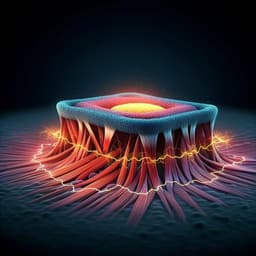
Bioink preparation: Cell-laden hydrogel was a fibrinogen-based composite (fibrinogen, gelatin, hyaluronic acid, glycerol in DMEM/high glucose), filtered sterile and mixed with cells. Sacrificial bioink was gelatin with HA and glycerol. Supporting bioink was thermoplastic polycaprolactone (PCL; Mw 43–50 kDa) for pillar anchors.
3D bioprinting: Custom multi-material bioprinter with pneumatic dispensing and temperature control printed cell-laden hydrogel, sacrificial hydrogel, and PCL in a layer-by-layer parallel pattern. Nozzle ~300 μm; typical dispensing speeds 90–160 mm/min; PCL extruded at ~95 °C. Printed PCL pillars anchored muscle bundles; sacrificial patterns were removed at 37 °C to create microchannels. Constructs were crosslinked in thrombin (20 U/mL) for 30–60 min, cultured overnight in growth medium, then switched to differentiation medium with aprotinin. For in vitro studies, constructs (~10×10×3 mm³) contained hMPCs alone or hMPCs+hNSCs at 300:1. For in vivo, constructs (~10×7×3.6 mm³) were fabricated at ~30×10^6 cells/mL and pre-differentiated 4–5 days before implantation.
In vitro assays: Live/dead confocal imaging for viability; immunofluorescence for MHC, βIIIT, GFAP, AChR; quantification of MHC+ myofiber density and length; counts of AChR clusters and NMJs per field. Calcium imaging (Fluo-4) with acetylcholine stimulation assessed synaptic function and calcium influx. Blinded image analysis with ImageJ.
Animal model and surgery: Male immunodeficient RNU rats (10–12 weeks) underwent creation of a standardized TA volumetric muscle loss: excision of ~40% mid-belly TA and ablation of EDL/EHL to prevent compensation. Constructs (after removal of PCL pillars) were implanted into the defect and covered by fascia and skin closure. Groups: sham, non-treated defect, MPC-only construct, and MPC+NSC construct (300:1). n=3 per group per time point (4 and 8 weeks), total n=24 rats.
In vivo functional testing: Under anesthesia, peroneal nerve was stimulated (100 Hz, 10 V, 0.1 ms) and peak isometric torque recorded with a dual-mode muscle lever system. Tetanic force normalized (N-mm/kg). TA muscles were harvested and weighed to calculate percent of contralateral TA.
Histology and immunofluorescence: Cryosections (6 μm) stained with H&E and Masson’s Trichrome for morphology and fibrosis (collagen area). Immunostaining for MHC and HLA to identify human-derived myofibers, NF/AChR/MHC and NF/AChR/HLA to assess NMJs and host–graft integration, and βIIIT/HLA for neuronal differentiation. Vascularization assessed by vWF and α-SMA double staining; vessel number and area quantified. Blinded quantification of MHC+ area, HLA+ myofibers, AChR clusters, NMJs per high-power field, and NMJ+ myofibers.
Statistics: Student’s t-test, one-way or two-way ANOVA with Tukey’s post hoc tests; data as mean±SD; significance at p<0.05.
Key Findings
- 2D co-culture optimization: An hMPC:hNSC ratio of 300:1 maximized myotube formation at day 10, with increased MyoD+ and myogenin+ cells, and enhanced myotube length, diameter, nuclei per myotube, and striation versus hMPC-only. Higher neural ratios (>300:1) suppressed myotube fusion. Increased AChR clustering and βIIIT/NF colocalization with AChRs on MHC+ myotubes indicated NMJ formation.
- 3D constructs in vitro: Day-1 cell viability was higher with neural integration (MPC+NSC 94.99±0.74%) versus MPC-only (85±2.20%). MHC+ myofiber density increased 1.71-fold and myofiber length increased in MPC+NSC constructs. hNSCs differentiated into GFAP+ glia and βIIIT+ neurons; βIIIT+ neurites contacted AChR clusters (pre-formed NMJs). Calcium imaging showed more cells with elevated intracellular calcium upon ACh stimulation in MPC+NSC constructs.
- In vivo muscle mass and function: Both bioprinted groups restored TA volume by 8 weeks versus severe atrophy in non-treated defects. TA muscle weight (% contralateral) in both MPC-only and MPC+NSC was not significantly different from sham at 8 weeks, with MPC+NSC showing earlier recovery by 4 weeks. Tetanic force at 8 weeks: sham 100.82±10.62 N-mm/kg vs MPC+NSC 97.79±14.44 N-mm/kg (p=0.980), indicating full functional restoration; MPC-only reached 71.42% of sham at 8 weeks and was significantly lower than MPC+NSC.
- Histology and myogenesis: MPC-only and MPC+NSC groups showed organized, aligned myofibers with reduced fibrosis versus non-treated. Implanted human cells (HLA+) contributed to MHC+ myofibers (MHC+/HLA+), with greater MHC+ and HLA+ myofiber area in MPC+NSC than MPC-only at both 4 and 8 weeks (p=0.001).
- Innervation: Both groups formed NMJs with host nerves, but MPC+NSC showed more AChR clusters and NMJs per field and more mature, pretzel-like NMJ morphology comparable to sham. NMJ+ myofiber percentages were not significantly different from sham in MPC+NSC by 8 weeks.
- Vascularization: vWF+/α-SMA+ vessel number and area were increased in both implanted groups versus non-treated, with no significant difference between MPC-only and MPC+NSC.
Overall, neural integration enhanced cell survival, myogenic differentiation, NMJ pre-patterning in vitro, accelerated innervation in vivo, and led to full restoration of muscle force by 8 weeks.
Discussion
The study addresses delayed innervation as a critical barrier to functional recovery of engineered muscle after volumetric loss. By integrating hNSCs with hMPCs at an optimized ratio (300:1), the constructs exhibited enhanced myogenesis, long-term survival, and pre-formed NMJs in vitro, likely mediated by neurotrophic factors and neurotransmitters that promote adhesion, proliferation, and differentiation. Pre-patterned AChR clusters facilitated rapid host nerve engagement post-implantation, increasing NMJ numbers and maturity to levels comparable to native muscle. Consequently, constructs restored TA muscle mass and achieved full functional recovery of tetanic force by 8 weeks, outperforming muscle-only constructs, which lagged in force restoration. While both implanted groups were similarly vascularized, the neural component specifically advanced innervation and myofiber maturation, demonstrating that neural-muscle crosstalk can expedite integration with host neural networks and improve functional outcomes in vivo.
Conclusion
Integrating neural cells into 3D bioprinted human skeletal muscle constructs supports long-term cell survival, enhances myogenic differentiation, and induces NMJ formation in vitro, which translates into accelerated innervation and restoration of muscle mass and function in a rat tibialis anterior volumetric defect model. NMJ-preformed constructs achieved muscle force comparable to sham by 8 weeks. This approach offers a promising therapeutic avenue for repairing extensive skeletal muscle defects. Future work should refine innervation mechanisms, evaluate contractile properties (twitch and tetanus) in vitro, develop clinically practical neural components (e.g., iPSC-derived neural cells or trophic factor delivery), enhance vascularization for larger constructs, and assess immune responses in immunocompetent models using autologous cells.
Limitations
- Clinical practicality of hNSC sourcing is limited; alternatives such as iPSC-derived neural cells or trophic factor delivery are needed for translation.
- The study used immunodeficient rats with human cells; host immune and inflammatory responses in immunocompetent settings remain to be characterized.
- Large-volume construct vascularization remains a challenge despite improvements; strategies to overcome diffusion limits are needed.
- In vitro assessments did not include direct measurements of construct contractility (twitch/tetanus), which should be evaluated in future studies.
- Small group sizes (n=3 per group/time point) may limit statistical power for some endpoints.
Related Publications
Explore these studies to deepen your understanding of the subject.