Medicine and Health
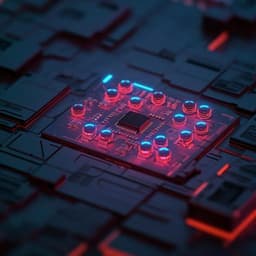
Miniaturized all-in-one microneedle device for point of care light therapy
H. Zhao, X. Wang, et al.
Discover the revolutionary Miniaturized all-in-one Light therapy Device (MiLD) designed for effective point-of-care treatment! This innovative device combines microneedles and an LED array to provide targeted light therapy with minimal side effects. Research conducted by Huiting Zhao, Xu Wang, Jiyuan Xiong, Guomin Liang, Xin Wu, Jiyu Xi, Yu Zhang, Zixi Li, Xiaoming Hu, and Zewen Wei shows promising therapeutic outcomes in both tissue removal and growth applications.
~3 min • Beginner • English
Introduction
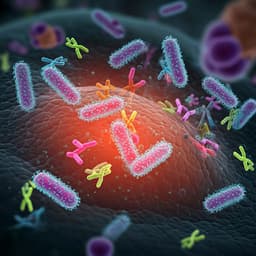
The study addresses limitations of conventional light therapies for superficial diseases, which typically rely on intravenous photosensitizer administration and direct surface illumination. These approaches lead to systemic photosensitizer accumulation with metabolic burden and phototoxicity, and require high irradiance (often 150–500 mW cm−2) to overcome stratum corneum losses, causing pain and tissue damage. Bulky, costly equipment further limits access and patient compliance for multi-visit treatments. The research question is whether a miniaturized, all-in-one microneedle-based device can transdermally co-deliver photosensitizer and therapeutic light directly to target tissue to maintain efficacy while reducing irradiance, eliminating circulatory photosensitizer, and enabling point-of-care use. The purpose is to develop and validate a battery-powered Miniaturized all-in-one Light therapy Device (MiLD) that integrates dual-function microneedles, LED light source, control circuitry, heat management, and battery, and to demonstrate its therapeutic effectiveness and reduced adverse effects in mouse models of photodynamic therapy (PDT) for port-wine stains (PWS) and photochemical tissue bonding (PTB) for wound repair.
Literature Review
The paper reviews current clinical light therapies that combine photosensitizers with light, noting improved outcomes (e.g., ALA improving epidermoid carcinoma therapy by 47%; verteporfin-mediated PDT as first-line for central serous chorioretinopathy; MAL-PDT for actinic keratosis). Standard practice uses intravenous photosensitizers and direct illumination, which causes systemic accumulation, ambient-light activation leading to skin/eye damage, and necessitates weeks of daylight avoidance. Direct illumination demands high irradiance to overcome stratum corneum, risking pain and tissue injury, and requires bulky hospital-based equipment. Transdermal delivery of photosensitizers has been explored using chemical enhancers (e.g., transfersomes) and physical methods (iontophoresis, microneedles) with reported high clearance rates in actinic keratosis. Transdermal delivery of therapeutic light is less mature; biodegradable polymer waveguides (PLA/PLGA) have been studied, but clinical effectiveness remains unconfirmed. The concept of simultaneous transdermal delivery of both photosensitizer and light has been proposed, but a full-function portable device achieving this for superficial disease treatment had not been realized prior to this work.
Methodology
Device design and fabrication: MiLD integrates five layers from bottom to top: (1) dual-function microneedle array for transdermal co-delivery of photosensitizer and light; (2) LED array (narrowband, 525 nm in this study) on a polyimide PCB; (3) graphene membrane for heat dissipation; (4) control module with MCU and Bluetooth for wireless control and PWM-based irradiance adjustment; (5) lithium battery. The assembled device measures 2.0 × 1.7 × 1.2 cm and weighs 3.6 g. The microneedle array comprises 400 needles (20×20, 500 µm spacing). Each microneedle has a dissolvable sodium hyaluronate (HA) tip (100 µm height) loaded with photosensitizer and a transparent polyvinyl alcohol (PVA) body (base width 300 µm, height 700 µm) that acts as a light guide after tip dissolution.
Fabrication process: A copper microneedle master (900 µm height, 300 µm width, 500 µm spacing) was machined; PDMS molds were cast and cured (80 °C, 30 min). Photosensitizer-loaded HA solution (0.2 g ml−1 HA) was cast and vacuumed (−0.9 bar, 30 min) into tips; excess was removed. PVA solution (15% w/v) was cast and vacuumed (−0.9 bar, 10 min) to form bodies; before solidification, a 525 nm LED array was coupled and left to solidify at room temperature for 48 h. The LED-coupled microneedle array was demolded and assembled with graphene, control module, and battery. Components were UV-sterilized prior to assembly. Microneedles were characterized by stereoscope and SEM.
Thermal management: A graphene membrane was incorporated; temperature reductions of 9.36–18.10 °C were quantified, maintaining 35.6–36.3 °C at 20 mW cm−2.
Control and operation: Wireless software presets disease-specific parameters; PWM control adjusted irradiance from 10 to 160 mW cm−2 as driving voltage increased from 27.9 to 38.8 V.
Insertion and delivery assessment: FITC-loaded HA tips were used to assess insertion depth via confocal microscopy and 3D reconstruction; HA tip dissolution was tested in 3% agarose.
Optical simulation: Monte Carlo models of mouse skin (stratum corneum 20 µm, epidermis 30 µm, dermis 150 µm; optical parameters in Supplementary Table 1) compared incident flux for MiLD-mediated illumination at 20 mW cm−2 vs direct illumination (20 and 80 mW cm−2). Incident flux profiles up to 200 µm depth were computed and integrated.
Animal studies: Female ICR mice under SPF conditions with dorsal skin-fold window chambers. PDT for PWS model: Five groups (n generally 6; Group 2 n=3) — (1) MiLD-HMME (0.75 µg) no light; (2) unloaded MiLD light 20 mW cm−2 for 15 min; (3) IV HMME 300 µg + direct light 20 mW cm−2 for 15 min; (4) IV HMME 300 µg + direct light 80 mW cm−2 for 15 min (positive control); (5) MiLD-HMME 0.75 µg + MiLD light 20 mW cm−2 for 15 min after 30 min diffusion. Vascular imaging daily for 5 days via window chamber; binary image analysis quantified vascular area.
Histology and inflammation: Three groups (n=1 for histology; n=3 for qRT-PCR) — control, direct illumination 80 mW cm−2, MiLD 20 mW cm−2; H&E staining for morphology and inflammation; qRT-PCR for IL1 mRNA normalized to GAPDH.
Pharmacokinetics: Three groups (n=6): control, IV-HMME 300 µg, MiLD-HMME 0.75 µg; blood collected post-administration; HMME quantified by LC/MS/MS with UHPLC XB-C18 column (MeOH/water 85/15, 0.2 ml min−1).
PTB wound repair: Six groups (n=3): (1) no treatment; (2) unloaded MiLD light 40 mW cm−2 for 20 min; (3) MiLD-RB 22.5 µg no light; (4) smear RB 0.05% + direct light 40 mW cm−2; (5) smear RB + direct light 110 mW cm−2; (6) MiLD-RB 22.5 µg + MiLD light 40 mW cm−2 for 20 min. Immediate bonding strength measured day 0 with a universal testing machine; wound area measured day 3 by ImageJ.
Statistics: Two-tailed unpaired Student’s t-test; p < 0.05 significant; data as mean ± SD. Ethical approval from BIT Animal Experimental Ethics Committee (SYXK-BIT-20211118020).
Key Findings
- Device integration and size: MiLD integrates microneedles, LED array, graphene heat spreader, control module, and battery into a 2.0 × 1.7 × 1.2 cm, 3.6 g unit enabling patch-to-cure operation and wireless control.
- Thermal management: Graphene membrane reduced temperature by 9.36–18.10 °C and maintained device surface at 35.6–36.3 °C during 20 mW cm−2 illumination.
- Microneedle performance: Arrays of 400 microneedles (500 µm spacing) with HA tips (100 µm) and PVA bodies (700 µm) achieved insertion depths of ~140 µm under gentle manual application; HA tips fully dissolved within 5 min in tissue surrogate; compression strength 24.178 N.
- Optical delivery: PWM control yielded 10–160 mW cm−2 irradiance (drive voltages 27.9–38.8 V). Monte Carlo simulations showed MiLD at 20 mW cm−2 produced incident flux within tissue similar to direct illumination (DI) at 80 mW cm−2 and far exceeding DI at 20 mW cm−2. Integrated incident flux from 0–200 µm depth: MiLD 20 mW cm−2 = 22.56 mW; DI 80 mW cm−2 = 20.31 mW; DI 20 mW cm−2 = 5.08 mW.
- PDT efficacy (PWS model): Groups 1–3 (photosensitizer only; light only 20 mW cm−2; IV HMME + DI 20 mW cm−2) showed no vessel damage, with vascular area increasing to ~159%, 145%, and 139% of baseline by day 5. Positive control Group 4 (IV HMME + DI 80 mW cm−2) reduced vascular area to ~8% by day 5. MiLD Group 5 (MiLD-HMME 0.75 µg + 20 mW cm−2) reduced vascular area to ~11% by day 5, achieving comparable efficacy with 60% lower irradiance and 400-fold lower photosensitizer dose.
- Tissue safety and inflammation: DI at 80 mW cm−2 caused epidermal thickening, broken dermal fibers, and inflammatory-cell infiltration; MiLD at 20 mW cm−2 markedly alleviated these changes. IL1 mRNA was significantly upregulated after DI 80 mW cm−2 but normalized in MiLD 20 mW cm−2.
- Pharmacokinetics: After IV 300 µg HMME, blood contained 63.29 µg HMME at 2 min; after MiLD transdermal delivery of 0.75 µg HMME, no HMME was detected in blood, indicating elimination of circulatory photosensitizer.
- PTB wound repair: Immediate bonding strengths were minimal without treatment (0.009 N) and modest with light-only (0.188 N), microneedle-only (0.208 N), or smear-RB + 40 mW cm−2 (0.337 N); significantly higher bonding occurred with smear-RB + 110 mW cm−2 and MiLD-RB + 40 mW cm−2 (exact values not specified but described as significantly higher). By day 3, wound areas: control 0.421 cm²; unloaded MiLD light 0.348 cm²; MiLD-RB no light 0.365 cm²; smear-RB + DI 40 mW cm−2 0.300 cm²; smear-RB + DI 110 mW cm−2 0.227 cm²; MiLD-RB + 40 mW cm−2 0.044 cm² (smallest area) at lower irradiance, avoiding high-irradiance damage.
- Comparative metrics (Table 1): Traditional PDT vs MiLD — photosensitizer dose 300 µg vs 0.75 µg; irradiance 80 vs 20 mW cm−2; therapeutic effect 92% vs 89%; light shielding needed >14 days vs none; device volume 189,840 cm³ vs 4.08 cm³; weight 22.5 kg vs 0.0036 kg.
Discussion
The MiLD addresses key barriers in light therapy for superficial diseases by co-delivering photosensitizer and therapeutic light directly into target tissue through dual-function microneedles. This bypasses the stratum corneum, increasing effective in-tissue incident flux and enabling a fourfold reduction in required irradiance relative to direct illumination. In PDT, MiLD achieved vessel ablation efficacy comparable to standard high-irradiance therapy while dramatically reducing both irradiance and photosensitizer dose, thereby minimizing light-induced tissue damage and eliminating systemic photosensitizer exposure. Histology and molecular assays corroborate reduced inflammation and absence of overheating-related gene dysregulation with MiLD parameters. In PTB, MiLD provided strong immediate tissue bonding and superior 3-day wound closure at lower irradiance, demonstrating applicability for promoting healthy tissue growth. The portable, battery-powered, wireless-controlled format simplifies operation and supports point-of-care deployment beyond centralized hospital settings. Collectively, these findings confirm that targeted transdermal co-delivery via microneedle light-guides can maintain or improve therapeutic outcomes while mitigating adverse effects and logistical burdens.
Conclusion
This work introduces a miniaturized, battery-powered, all-in-one microneedle light therapy device (MiLD) that co-delivers photosensitizer and therapeutic light in situ, enabling patch-to-cure, point-of-care treatment. In mouse models, MiLD achieves PDT efficacy comparable to standard care with 60% lower irradiance and 400-fold lower photosensitizer dose, eliminates circulatory photosensitizer, and markedly reduces light-induced tissue damage and inflammation. MiLD also enhances PTB-mediated wound repair at lower irradiance, indicating versatility for therapies requiring tissue regeneration. The device’s modular design allows simple wavelength and irradiance adjustments (e.g., adapting to 630 nm for ALA/MAL-based PDT) and scalability of treatment area by redesigning the microneedle array. Future work should evaluate long-term safety, durability, and efficacy in larger animals and humans, optimize dosing/irradiance protocols across indications, expand array footprints for larger lesions, and integrate closed-loop sensing for personalized dosimetry.
Limitations
Findings are based on preclinical mouse models; clinical efficacy and safety remain to be established. Optical simulations and measurements focused on shallow tissue depths (≤200 µm) suitable for superficial diseases; performance in thicker or varied skin types was not reported. Histological analysis used small sample sizes (e.g., n=1 for H&E groups), limiting statistical power. Experiments primarily used a single wavelength (525 nm) and specific photosensitizers (HMME, Rose Bengal); generalizability to other wavelengths/agents requires validation. Thermal and mechanical characterizations were performed under selected conditions; long-term wear, repeated-use durability, and broader environmental factors were not assessed.
Related Publications
Explore these studies to deepen your understanding of the subject.