Medicine and Health
Microbiota-gut-brain axis in neurodegenerative diseases: molecular mechanisms and therapeutic targets
C. Chen, G. Wang, et al.
This review synthesizes evidence that the microbiota‑gut‑brain axis modulates neuroinflammation, blood‑brain barrier integrity, protein misfolding, and neuronal homeostasis via microbial metabolites such as short‑chain fatty acids, tryptophan derivatives, and bile acids, and explores microbiota‑targeted therapies. Research was conducted by Ce Chen, Guo-qing Wang, Dai-di Li, and Feng Zhang.
~3 min • Beginner • English
Introduction
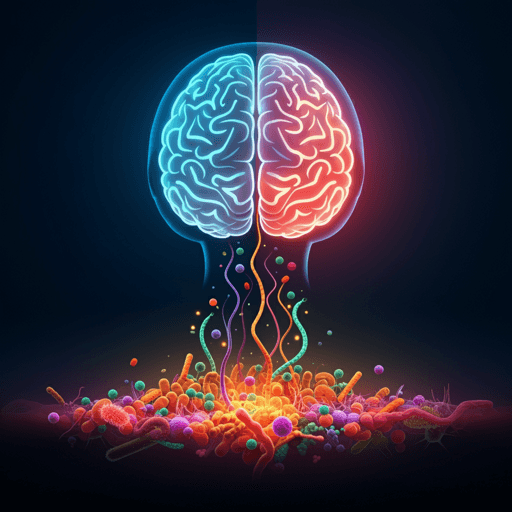
Neurodegenerative diseases (NDDs)—including Alzheimer’s disease (AD), Parkinson’s disease (PD), Huntington’s disease (HD), and amyotrophic lateral sclerosis (ALS)—are characterized by progressive neuronal loss leading to cognitive and/or motor deficits and impose a major global health burden. Emerging research links gastrointestinal abnormalities and gut microbiome alterations to prodromal and clinical stages of these disorders, suggesting that perturbations in the microbiota-gut-brain axis (MGBA) may contribute to disease initiation and progression. The MGBA is a bidirectional network integrating gut microbiota, intestinal barrier and immune system, the enteric nervous system and vagus nerve, systemic immune and endocrine signaling (including the HPA axis), and CNS interfaces such as the blood–brain barrier and microglia. Stress and CNS pathology can alter gut function and microbial ecology, creating feedback loops that exacerbate systemic and neuroinflammation. This review synthesizes current knowledge on MGBA components and communication routes (neural, immune/inflammatory, endocrine/metabolic, and microbial metabolites), delineates mechanistic links to neurodegeneration (neuroinflammation, BBB integrity and metabolism, protein misfolding, epigenetic and neuronal signaling), summarizes disease-specific microbiome alterations in AD, PD, MS, and ALS, and evaluates microbiota-targeted therapeutic strategies (diet, probiotics/synbiotics, fecal microbiota transplantation, postbiotics, and pathway-targeted drugs). The goal is to clarify how the MGBA shapes neurodegenerative processes and to identify translational opportunities and challenges for precision, microbiome-informed interventions.
Literature Review
This narrative review integrates preclinical and clinical literature on the microbiota-gut-brain axis across major neurodegenerative diseases. It details: (1) MGBA components and four principal communication pathways (neural/vagal, immune/inflammatory, endocrine/metabolic, and microbial neurotransmitters/metabolites); (2) mechanistic links between gut dysbiosis and neurodegeneration, including chronic neuroinflammation, BBB dysfunction and metabolic imbalance, protein misfolding/aggregation, and epigenetic/neurotransmission changes; (3) disease-specific microbiome and metabolome alterations and their putative roles in AD (reduced diversity, fewer SCFA producers, altered bile acids, links to amyloid/tau pathology), PD (loss of Prevotellaceae and SCFA producers, enrichment of Akkermansia and Enterobacteriaceae, α-syn propagation hypotheses, levodopa-metabolizing bacteria), MS (Th17/Treg imbalance linked to microbial profiles, reduced butyrate producers, decreased AhR ligands), and ALS (heterogeneous dysbiosis, potential benefits of Akkermansia-derived nicotinamide, SCFA support); and (4) interventional evidence spanning diet (Mediterranean/MIND, ketogenic trials), probiotics/synbiotics (improvements mainly in GI and inflammatory markers), fecal microbiota transplantation (mixed clinical outcomes, donor/engraftment effects), postbiotics (SCFAs, bile acids, vitamins, tryptophan metabolites), and targeted microbial pathway modulation (e.g., enzyme inhibitors, phage therapy). The review contextualizes findings with mechanistic models, multi-omics studies, and selected randomized trials, highlighting variability, potential biomarkers, and the need for personalized approaches.
Methodology
This is a narrative (non-systematic) review synthesizing recent preclinical and clinical studies up to 2025 on the microbiota-gut-brain axis in neurodegenerative diseases. No explicit systematic search strategy, inclusion/exclusion criteria, or PRISMA flow diagram are reported. Evidence is drawn from mechanistic experiments (germ-free/gnotobiotic and transgenic animal models), multi-omics human studies (microbiome, metabolome, imaging, CSF), observational cohorts, and interventional trials (dietary patterns, probiotics/synbiotics, fecal microbiota transplantation, and postbiotics). The authors summarize representative findings, figures, and tables (including clinical trial overviews) to illustrate mechanisms, disease-specific alterations, and therapeutic implications.
Key Findings
- MGBA mechanisms: Gut microbes influence the CNS via neural (vagus/ENS), immune (cytokines, T cell polarization), endocrine/metabolic (gut hormones, HPA axis), and microbial metabolite pathways (SCFAs, bile acids, tryptophan derivatives, neurotransmitters). Dysbiosis can drive systemic and neuroinflammation, impair barrier integrity, disrupt metabolism, and modulate protein aggregation and epigenetics.
- Immune-neuroinflammation: Increased gut permeability allows MAMPs (e.g., LPS) to activate TLR-mediated microglial responses; dysbiosis skews Th17/Treg balance. SCFAs promote Tregs and anti-inflammatory microglial states; tryptophan-derived AhR ligands modulate astrocyte/microglia activity.
- BBB and metabolic homeostasis: Butyrate strengthens intestinal/BBB barriers and acts as an epigenetic modulator; altered bile acid pools and amino acid metabolism link gut changes to CNS metabolism and microglial function. Potentially detrimental metabolites (e.g., TMAO, ammonia) are elevated with dysbiosis.
- Proteinopathies: Bacterial amyloids (e.g., curli) may cross-seed host proteins; α-syn pathology may spread from gut via the vagus. Microbial signals influence autophagy/proteostasis (butyrate, acetate) and microglial phagocytosis of Aβ.
- Epigenetics/neuronal signaling: SCFAs (butyrate/acetate) alter histone acetylation and gene expression (BDNF, plasticity); bile acids (TGR5/FXR) and SCFA receptors (FFAR2/3, HCAR2) link metabolites to neuronal and glial signaling.
- Alzheimer’s disease: Reduced diversity and SCFA producers (e.g., Faecalibacterium, E. rectale), increased pro-inflammatory taxa (e.g., Escherichia/Shigella); altered bile acids; reduced fecal SCFAs; antibiotic/microbiome manipulations modulate amyloidosis in models; probiotics show modest cognitive/inflammatory benefits in small RCTs.
- Parkinson’s disease: Depletion of Prevotellaceae/SCFA producers; enrichment of Akkermansia and Enterobacteriaceae; low fecal SCFAs and increased intestinal permeability; gut bacteria can metabolize levodopa, influencing therapy. Clinical interventions show mixed efficacy: probiotics improve constipation and may modestly impact motor scores; RCT evidence for FMT is mixed with at least one multicenter RCT not meeting its primary endpoint and higher GI adverse events in FMT vs placebo (~53% vs ~7%).
- Multiple sclerosis: Lower butyrate producers (e.g., Faecalibacterium), higher pro-inflammatory taxa (e.g., Akkermansia); enhanced Th17 and reduced Tregs linked to microbiota; propionate supplementation in patients increases Tregs and associates with reduced relapses; probiotics reduce inflammatory cytokines in small RCTs; FMT early trials suggest safety with exploratory benefits.
- Amyotrophic lateral sclerosis: Heterogeneous dysbiosis; in mouse models, certain microbes (e.g., Akkermansia) provide nicotinamide and slow disease; SCFA-supporting strategies show neuroprotective signals; an RCT of FMT in sporadic ALS showed no ALSFRS-R benefit vs placebo but improved constipation/mood; dietary hypercaloric strategies may be beneficial.
- Therapeutic landscape: Diet (Mediterranean/MIND, fiber/polyphenols) fosters eubiotic microbiomes and SCFA production; probiotics/synbiotics have favorable safety with variable, context-dependent benefits; FMT shows biological effects but inconsistent clinical outcomes due to donor-, protocol-, and engraftment-variability; postbiotics (butyrate, propionate, bile acids, vitamins) and pathway-targeted approaches (enzyme inhibitors, phages) are promising adjuncts.
- Translational needs: Personalization with baseline microbiome/metabolome stratification, harmonized mechanistic biomarkers (SCFAs, bile acids, barrier/immune markers), optimized donor/route/dose for FMT, and combination (induction-maintenance) designs are emphasized.
Discussion
The review argues that MGBA dysregulation contributes to neurodegeneration through converging mechanisms—chronic immune activation, barrier dysfunction, metabolic and endocrine disruption, protein misfolding, and altered neuronal signaling. By integrating animal and human evidence across AD, PD, MS, and ALS, it addresses how disease-specific microbiome patterns and metabolites can shape CNS pathology and symptomatology. The findings highlight the MGBA as a multi-target therapeutic entry point: restoring eubiosis and beneficial metabolite profiles can attenuate neuroinflammation, improve proteostasis and synaptic plasticity, and support neuronal resilience. However, inter-individual variability, context-dependent effects of taxa/metabolites, and inconsistencies in clinical outcomes underscore the need for personalized, biomarker-guided interventions and rigorous, standardized trial designs. The MGBA framework reframes neurodegenerative diseases as systemic disorders and supports combining CNS-directed agents with gut-focused therapies for additive or synergistic benefits.
Conclusion
This review consolidates mechanistic, translational, and clinical evidence that the microbiota-gut-brain axis materially contributes to the pathogenesis and progression of neurodegenerative diseases. Key contributions include: (i) a mechanistic map linking gut microbes and metabolites to neuroinflammation, BBB integrity, proteostasis, and epigenetic/neurotransmission; (ii) disease-specific microbiome signatures in AD, PD, MS, and ALS; and (iii) a critical appraisal of microbiota-targeted strategies (diet, probiotics/synbiotics, FMT, postbiotics, and precision modulators). The authors advocate for next steps centered on multi-omics integration, longitudinal cohorts to establish temporality/causality, gnotobiotic/mechanistic models to pinpoint effectors, and clinical trials with standardized products, co-primary mechanistic endpoints, and patient stratification. Future directions include defined microbial consortia and engineered strains, targeted inhibition of harmful microbial pathways, and personalized, combination regimens that align diet, live biotherapeutics, and metabolite/drug adjuncts to maximize efficacy and durability.
Limitations
- Narrative review without a predefined systematic search strategy or PRISMA methodology; potential selection bias in cited literature.
- Heterogeneity across studies (populations, diets, medications, microbiome sequencing/analytics, and outcome measures) limits cross-study comparability and can yield conflicting results.
- Causality remains difficult to establish in humans; many associations are correlative, and effects may be bidirectional (disease altering microbiome vs microbiome contributing to disease).
- Clinical trial evidence is still limited and variable, with modest effect sizes, donor- and protocol-dependent outcomes for FMT, and context/strain-dependent efficacy for probiotics.
- Lack of standardized product characterization (strain identity, dose/viability), biomarker panels, and engraftment measures hampers reproducibility and regulatory evaluation.
- Inter-individual variability (genetics, environment, comorbidities, medications) complicates generalizability and necessitates personalized approaches.
Related Publications
Explore these studies to deepen your understanding of the subject.