Medicine and Health
Mechanical Ventilation Induces Neutrophil Extracellular Trap Formation
C. Yildiz, N. Palaniyar, et al.
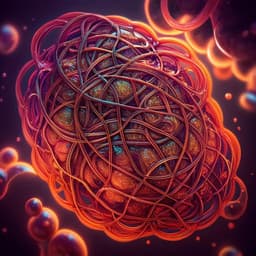
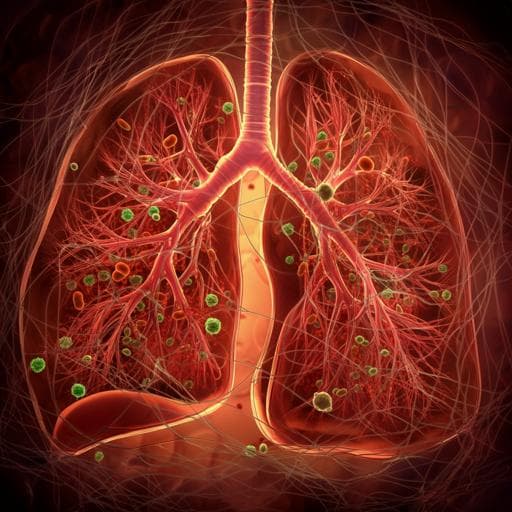
Mechanical ventilation is essential in intensive care but can cause ventilator-induced lung injury (VILI). Neutrophil infiltration is central to VILI pathogenesis, and neutrophils can injure tissue via proteases, reactive oxygen species, and proinflammatory mediators. Neutrophil extracellular traps (NETs)—genomic DNA decorated with granule proteins—trap and kill pathogens but have been implicated in tissue damage and autoimmune disease, and have been detected in lung injury contexts such as transfusion-related acute lung injury, asthma, and pneumonia. NET formation (NETosis) involves histone citrullination and chromatin decondensation via ROS-dependent and -independent pathways. Mechanical ventilation is associated with increases in potential NETosis inducers (e.g., IL-8, IL-1β, HMGB1) in lungs. The research question was whether NETosis occurs during VILI and whether NETs contribute to lung injury. The authors hypothesized that a two-hit model (lipopolysaccharide to recruit neutrophils plus injurious high tidal volume ventilation) would induce NETs and that targeting NETs (with DNase I) or blocking candidate inducers (IL-1β, HMGB1) would mitigate injury.
Prior studies indicate that neutrophil depletion can attenuate ventilator-associated increases in extravascular lung protein and improve oxygenation, underscoring neutrophils' role in VILI, although global depletion is not clinically viable. NETs have been linked to tissue damage and autoimmunity and have been detected in lung microvasculature in transfusion-related acute lung injury, where targeting NET components was protective in mice. NETs have also been found in human asthmatic airways and in murine pneumonia models. HMGB1 levels rise during mechanical ventilation in humans and animal models and can promote NETosis via TLR4, especially with LPS. Cytokines such as IL-1β, TNFα, MIP-2, and KC have been associated with VILI and can induce NETosis under some conditions. The inflammasome contributes to VILI and promotes IL-1β production. Together, these observations suggest a potential role for NETs in ventilator-associated lung pathology.
Design: Experimental two-hit mouse model of lung injury. Animal ethics: Approved by the Hospital for Sick Children Research Institute (Toronto) in accordance with Canadian Council on Animal Care guidelines. Animals: Adult C57BL/6 mice (20–25 g). Experimental groups (n=10/group in primary series): PBS/spontaneous ventilation (SV); LPS/SV; PBS/low tidal volume ventilation (LV); PBS/high tidal volume ventilation (HV); LPS/LV; LPS/HV. Pretreatment: Intratracheal LPS (E. coli O111:B4), 5 µg in PBS, followed by 200 µl air; or PBS vehicle. Two hours later, tracheotomy and mechanical ventilation on a flexiVent ventilator (room air, volume-controlled). Ventilation protocols: HV (injurious): RR 45/min, VT 20 ml/kg, PEEP 0 cm H2O; LV (protective): RR 135/min, VT 10 ml/kg, PEEP 2 cm H2O. SV controls: anesthetized, intubated, no mechanical ventilation, sacrificed 6 h post-instillation. Supportive care: Normothermia (37°C), subcutaneous lactated Ringer’s 300 µl at start, maintenance anesthesia (pancuronium 0.1 mg hourly; ketamine 26.67 mg/kg/h; xylazine 6.67 mg/kg/h, intraperitoneal), hourly recruitment maneuvers to 30 cm H2O for 5 s. Measurements: Quasistatic compliance (pressure-volume loops) and dynamic compliance (snapshot perturbation). At 4 h of ventilation (6 h post-instillation), arterial blood gas from carotid artery; lungs perfused and BAL performed (3×700 µl HEPES-buffered saline). BALF stored at −80°C; cells stained and differentials counted. Interventions: DNase I series (n=20/group): Intratracheal Dornase alfa (25 µl of 1 mg/ml) vs vehicle (8.77 mg/ml NaCl, 0.15 mg/ml CaCl2), administered twice immediately after intubation (each followed by 700 µl air); all subjected to LPS/HV two-hit protocol. Pharmacologic blockade series (n=6/group): Vehicle; glycyrrhizin (10 mg/kg i.p., 10 min pre-ventilation) to inhibit HMGB1; anakinra (IL-1 receptor antagonist) 10 mg/kg intratracheal at LPS instillation plus 10 mg/kg i.v. at start of ventilation; all with LPS/HV protocol. Assays: BALF DNA by PicoGreen; BALF protein by BCA assay. Western blot on BALF for citrullinated histone-3 (Cit-H3), myeloperoxidase (MPO), and HMGB1. Cytokines in BALF by Milliplex multiplex (IL-1β, IL-6, KC, GM-CSF, G-CSF, TNFα, MIP-2, MCP-1). Lung cryosections (10 µm) prepared for immunofluorescence: anti–Cit-H3 staining with confocal imaging and DAPI colocalization. Histology: Formalin inflation fixation at 20 cm H2O, H&E staining; blinded morphometry (tissue fraction, mean linear intercept). Statistics: Mean ± SEM; two-group comparisons by t test or Mann–Whitney; multiple groups by two-way ANOVA or ANOVA on ranks with appropriate post hoc tests; Fisher exact test for Cit-H3 detectability; significance threshold P<0.05.
• LPS recruited neutrophils to airways without altering macrophage counts, increasing total inflammatory cells; HV alone did not significantly increase neutrophil recruitment. • NETosis required both hits: Cit-H3 was strongly detectable predominantly in the LPS + HV group (9/10 animals) versus 3/9 in LPS + LV, 1/9 in PBS + HV, and none in PBS + LV (HV P=0.002; LPS P=0.04, Fisher exact). • BALF DNA was significantly increased in LPS + HV over all other groups (e.g., 0.4±0.07 µg/ml, P<0.05 vs all others, n=10/group). • Injurious ventilation worsened lung mechanics and oxygenation: HV reduced static and dynamic compliance versus LV; both LPS pretreatment and HV contributed to decreased static compliance with significant interaction; BALF protein increased with both factors. Arterial oxygenation was lower in HV versus LV, trending lower with LPS. • Potential inducers: BALF HMGB1 increased with mechanical ventilation (e.g., 0.91±0.138 vs 0.60±0.095 arbitrary units in HV vs LV contexts). IL-1β, MCP-1, IL-6, and MIP-2 were highest in LPS + HV; TNFα, KC, and G-CSF were primarily LPS-driven with little HV contribution. • DNase intervention (LPS + HV model): Reduced NET markers—BALF DNA from 0.88±0.135 to 0.23±0.038 µg/ml (P<0.001) and Cit-H3 from 1,824±403 to 443±170 arbitrary units (P<0.01)—without changing BALF cell counts. DNase attenuated the decrement in static compliance (P=0.003), but did not improve blood gases, BALF protein, BALF MPO, or histologic tissue fraction. • Pharmacologic blockade: Neither HMGB1 inhibition (glycyrrhizin) nor IL-1 receptor blockade (anakinra) reduced NETs (Cit-H3 or DNA), improved compliance, or altered blood gases/BALF protein compared with vehicle.
This study demonstrates that NETosis occurs in a two-hit VILI model only when neutrophil recruitment by LPS is followed by injurious high tidal volume ventilation. The presence of Cit-H3 and increased extracellular DNA in BALF, together with immunofluorescent colocalization of Cit-H3 and DNA in alveoli, supports NET release into distal airspaces. Elevations of IL-1β and HMGB1 in the LPS + HV condition parallel NET formation, suggesting these mediators may contribute; however, blockade of either HMGB1 or IL-1 signaling alone was insufficient to prevent NETosis or protect the lung, implying redundant or multifactorial induction pathways. DNase I effectively eliminated NET markers and improved lung mechanics (reduced compliance loss), but did not ameliorate other injury indices (oxygenation, protein leak, inflammatory burden, or morphometric injury), indicating a limited pathogenic role for NETs in this LPS-primed VILI model. The findings contrast with models such as transfusion-related acute lung injury or single-hit high-pressure VILI where targeting NETs or elastase provided broader protection, highlighting model-dependent contributions of NETs. Overall, while NETs form during VILI and can influence mechanical properties, they are not a dominant driver of tissue injury under the current experimental conditions.
A two-hit mouse model (LPS pretreatment plus injurious ventilation) induces robust pulmonary NETosis, associated with elevated IL-1β and HMGB1. Intratracheal DNase I clears NETs and improves lung compliance but does not reduce inflammation, permeability, or gas exchange impairment, supporting a limited role of NETs in the pathogenesis of LPS-primed VILI. Pharmacologic inhibition of IL-1 or HMGB1 alone does not prevent NET formation. Future work should delineate upstream mechanotransduction pathways driving NETosis in VILI, assess combinatorial blockade of NET inducers, and explore context-dependent benefits of NET-targeted therapies across diverse VILI phenotypes and in infection-free versus infection-primed settings.
• The two-hit design (LPS priming plus HV) may not generalize to all VILI contexts; NET contributions may differ in single-hit or more severe ventilation strategies. • Short experimental duration (4 h ventilation) may limit detection of later pathophysiologic effects or therapeutic benefits. • Pharmacologic blockade targeted single mediators (IL-1, HMGB1); redundancy among NET inducers could mask effects. • DNase I was delivered intratracheally; systemic effects on circulating NETs were not assessed and may differ from intraperitoneal or intravenous delivery in other models. • Some outcomes (e.g., compliance improvement) could reflect changes in secretion viscosity rather than reduced structural injury. • Quantification of some markers used arbitrary units and detectability thresholds, which may limit cross-study comparisons.
Related Publications
Explore these studies to deepen your understanding of the subject.