Medicine and Health
Intelligent drugs based on notch protein remodeling: a defensive targeting strategy for tumor therapy
Y. Sun, Y. Lu, et al.
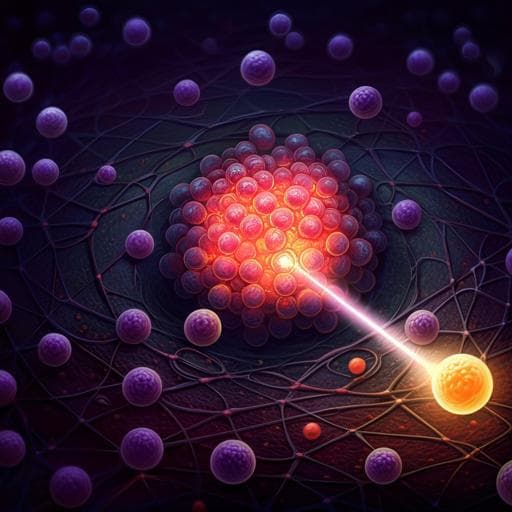
Systemically administered anticancer drugs face multiple biological barriers (intravascular, endothelial, extracellular matrix) that prevent sufficient accumulation at tumor sites and lead to extensive distribution in healthy tissues, causing adverse effects. Endostatin, despite efficacy across several cancers, predominantly accumulates in normal tissues (over 90–95%), with documented cardiotoxicity. Conventional targeting platforms, such as antibody-drug conjugates (ADCs) and cellular carriers, only partially mitigate off-target effects and often cannot overcome chemotactic and barrier-penetration challenges; moreover, cytokine similarities in non-tumor diseases risk off-target homing. The authors propose a defensive targeting paradigm: rather than maximizing lesion concentration, prevent drug presence in healthy tissues by enabling therapy to activate only upon direct tumor recognition. Leveraging the modularity of the Notch pathway—where the extracellular (ligand recognition) and intracellular (transcriptional) domains can be swapped while retaining a functional core—the study engineers MSCs to couple tumor recognition (Her2-affibody) to a transcriptional response (GAL4-VP64) that induces therapeutic protein production (endostatin). This establishes a logical linkage between tumor contact and on-demand drug deployment.
Prior work shows that biological barriers hinder effective delivery (e.g., high interstitial pressure), and tissue-specific targeting strategies often result in off-target exposure. ADCs can increase affinity but lack chemotaxis and barrier penetration. Cell-based carriers can home to tumors via chemokine receptors but may mis-home due to shared cytokines in other pathologies (e.g., CCL4 in myocarditis). The Notch signaling pathway offers a customizable, modular, tension-dependent activation mechanism: replacing Notch extracellular and intracellular domains with alternative recognition and transcriptional modules (synthetic Notch/synNotch) enables programmable cell sensing and response. Literature supports synNotch-CAR approaches improving specificity and persistence in solid tumors and indicates that MSCs have tumor-homing capacity while evading immunosuppression better than T cells in certain contexts. These insights motivate engineering MSCs with synNotch-like circuits to conditionally release therapeutics only upon direct tumor contact.
Ethics: Human Her2-positive breast cancer samples (IHC 3+) obtained with informed consent and ethics approval. Animal studies approved by Xinxiang Medical University; female Balb/c and Balb/c nude mice (6–8 weeks) housed under SPF conditions; randomization to cages, investigator-blinded; no statistical power calculation; no data exclusions. Cells: MSCs from Zhongyuan Stem Cell Research Institute; cell lines included BT474, Skov3, 293T, BJ, L02, Svog, HUVEC, AC16; lines authenticated and mycoplasma-free. Select lines were GFP-labeled via lentivirus. Construct design and generation of iMSCEndostatin: A recognition receptor retained the Notch1 core (Ile1427–Arg1752) with extracellular Her2-affibody and intracellular GAL4-VP64 (Affibody–Notch core–GAL4-VP64), including CD8a signal peptide (MALPVTALLLPLALLLHAARP) and C-myc tag (EQKLISEEDL). The response cassette used five Gal4 UAS sites upstream of a minimal CMV promoter driving endostatin, with a BFP tag, and in most assays an IRES-mCherry for co-expression reporting. Plasmids: pLVX-Affibody-Notch(core)-GAL4-VP64 (recognition) and pHR-Gal4/UAS-Endostatin-IRES-mCherry-PGK-BFP (response). Lentiviral transduction integrated both cassettes into MSCs to generate iMSCEndostatin. Immunostaining and Western blot: Standard permeabilization and blocking; primary antibodies included anti-Her2, anti-MMP-2, anti-MMP-9 for tissues, and anti-c-Myc for constructs; WB antibodies included c-Myc, Cyclin B1, CDK2, PCNA, GAPDH. Appropriate HRP-conjugated secondary antibodies used. In vitro tumor recognition assays: Co-culture iMSCEndostatin with Her2+ tumor cells (BT474-GFP, Skov3-GFP) and with non-tumor cells (293T-GFP, BJ-GFP, L02-GFP, Svog-GFP, HUVEC-GFP, AC16-GFP) for 24 h; analyze activation by confocal microscopy, live imaging, and flow cytometry. mCherry served as activation reporter (via IRES with endostatin). Endostatin production and secretion assays: Time-course co-cultures of iMSCEndostatin with Skov3-GFP on fibronectin for 15 min, 12 h, 24 h, 36 h, 48 h; fixation and fluorescence imaging to monitor mCherry accumulation (proxy for endostatin expression). Culture supernatants were assayed by microplate reader for mCherry fluorescence at specified time points and every 4 h post-full activation. For direct visualization of secretion, an endostatin–mCherry fusion was constructed (mCherry at the N-terminus in a secretion-competent endostatin with restored signal peptide) and imaged by confocal and 3D reconstruction; PBS washes distinguished extracellular secreted signal. ELISA quantified endostatin: MSCs or iMSCEndostatin were co-cultured with Skov3-GFP for 48 h, then sorted and reseeded 24 h; endostatin measured (subtracting naïve MSC background to account for collagen XVIII cross-reactivity). Angiogenesis-related assays: Conditioned media prepared by co-culturing iMSCEndostatin with Skov3 (activated) or with AC16 cardiomyocytes (unactivated) for 48 h, then concentrated 5-fold. HUVEC assays: CCK-8 viability after 48 h in conditioned media; CD105 expression by flow cytometry; proliferation proteins (c-Myc, Cyclin B1, CDK2, PCNA) by WB. Tube formation assay: HUVECs on Matrigel with control, unactivated, or activated conditioned media; imaging and quantification (covered area, branching points, total tube length, total tubes). Matrigel plug assay: Matrigel with bFGF plus conditioned media implanted subcutaneously in nude mice (n=3 per group); after 9 days, CD34 immunofluorescence assessed neovascularization. In vivo tumor models and therapy: Emt-6 cells were transduced to express human Her2 and GFP. Lung metastasis model: 2×10^5 Emt-6-GFP IV; at day 3, 3×10^6 iMSCEndostatin IV (n=5); organs collected 48 h later for confocal imaging of activation. Solid tumor model: 1×10^6 Emt-6-GFP subcutaneous; on day 11, 3×10^6 iMSCEndostatin IV (n=5); tumors collected 48 h later for imaging. Therapeutic study: 1×10^6 Emt-6 subcutaneous; groups (n=5): control (PBS), MSC, iMSCEndostatin (without mCherry); IV administrations on days 4, 7, 10; on day 14, tumor volume and weight measured and CD34 staining performed. Cardiotoxicity assessment: On day 14, ECG, serum myocardial enzymes (CK-MB, alpha-HBDH, LDH), and HE staining of hearts were performed for control, MSC, and iMSCEndostatin groups. Statistics: SPSS 8.0; data as mean ± SD; cell experiments at least triplicate; Dunnett’s test for comparisons among ≥3 groups; two-sided p<0.05 considered significant.
- Engineering: An MSC-based intelligent drug (iMSCEndostatin) was created using a Notch1-core-based synthetic receptor with a Her2-affibody recognition domain and GAL4-VP64 transcriptional effector linked to a Gal4/UAS-driven endostatin secretion cassette, enabling logical coupling of tumor recognition to therapeutic production.
- Specific recognition: iMSCEndostatin robustly recognized Her2+ tumor cells (BT474, Skov3) in co-culture, activating only upon tumor contact; unactivated cells were observed away from tumors. Flow cytometry confirmed selective activation. In macroscopic fields, deployment of endostatin was restricted to tumor areas.
- Discrimination from normal cells: No activation occurred when co-cultured with non-tumor human cell lines (293T, BJ, L02, Svog) or with cardiac-related cells (HUVEC endothelial cells, AC16 cardiomyocytes), supporting a defensive strategy that avoids drug presence in healthy tissues.
- Endostatin production/secretion kinetics: iMSCEndostatin began producing endostatin within ~12 h after recognizing Her2+ cells, peaking at ~48 h. After full activation, secretion into media was steady with similar amounts released every 4 h. Quantitatively, approximately 0.62 pg endostatin was produced per 5×10^4 activated iMSCEndostatin cells over 24 h (ELISA, background-subtracted). Confocal and 3D imaging visualized extracellular endostatin deposits around tumors.
- Anti-angiogenic activity in vitro: Conditioned media from activated iMSCEndostatin reduced HUVEC viability (CCK-8), significantly decreased CD105 expression (flow cytometry; corroborated by WB), and lowered proliferation markers (c-Myc, Cyclin B1, CDK2, PCNA). Tube formation metrics (covered area, branching points, total tube length, total tubes) were significantly reduced versus control and unactivated conditions. In matrigel plug assays in vivo, CD34+ area was significantly reduced in the activated iMSCEndostatin group.
- In vivo recognition and efficacy: In both lung metastasis and solid tumor models, iMSCEndostatin activated within tumors, with few tumor cells sufficient to trigger activation. Therapeutic administration (days 4, 7, 10) significantly reduced tumor volume and weight and decreased intratumoral vascular density (CD34) compared with control and naïve MSC groups (n=5 per group).
- Safety (cardiotoxicity): No significant differences were observed among groups in heart histology (HE), serum CK-MB, alpha-HBDH, LDH, ECG patterns, or heart rate, indicating no detectable cardiotoxicity under treatment conditions.
The study demonstrates a defensive targeting concept: by programming MSCs with a modular Notch-core-based synthetic receptor, therapeutic payload production (endostatin) occurs only upon direct contact with Her2+ tumor cells, minimizing exposure in healthy tissues. This approach addresses limitations of conventional targeting strategies that still leave substantial drug in non-tumor compartments due to biological barriers. The Notch-core’s tension-dependent activation confers contact-dependent specificity, reducing risks of remote, cytokine-mediated off-target activation and leakage. Functionally, iMSCEndostatin showed precise tumor recognition, selective activation, and sustained, periodic secretion of an anti-angiogenic payload, achieving inhibition of endothelial proliferation and angiogenesis in vitro and reduced tumor growth and vascularization in vivo, with no observed cardiotoxicity. The system’s modularity suggests adaptability: different recognition domains could target diverse tumor antigens, and response modules could drive alternative therapeutics. Moreover, orthogonal transcription systems could enable multiplexed programs for more complex logic and enhanced safety. Collectively, the findings validate that restricting drug deployment to lesions can lock therapeutic toxicity within tumors and reduce systemic side effects.
This work introduces iMSCEndostatin, an MSC-based intelligent drug that couples synNotch-like tumor recognition (Her2-affibody) to inducible secretion of endostatin, embodying a defensive targeting strategy. It selectively activates at Her2+ tumor sites, discriminates against normal cells, produces and secretes endostatin with defined kinetics, inhibits angiogenesis, and suppresses tumor growth in vivo without detectable cardiotoxicity. The platform’s modular design enables reprogramming of both inputs (tumor antigens) and outputs (therapeutic payloads), supporting personalized and multiplexed therapies. Future research should expand to additional tumor targets and payloads, optimize activation kinetics and secretion rates, evaluate long-term persistence and immunogenicity, implement multi-input safety logic, and conduct comprehensive preclinical toxicology and biodistribution studies to advance toward clinical translation.
- Scope limited to Her2+ models (BT474, Skov3, engineered Emt-6); generalizability to other tumor types and heterogeneous antigen expression remains to be shown.
- Activation kinetics are relatively slow (onset ~12 h, peak ~48 h), which may limit applicability in rapidly progressing contexts.
- Quantified endostatin output per cell is low on a per-cell basis; scaling to therapeutic levels relies on large cell numbers and persistence, which were not fully optimized.
- Animal studies used small cohorts (n=5) without a priori power calculations; longer-term efficacy, biodistribution, and safety (including immunogenicity of synthetic receptors and secreted proteins) were not extensively characterized.
- Normal tissue off-target activation was tested in selected cell types; comprehensive profiling across diverse tissues and inflammatory conditions is still needed.
Related Publications
Explore these studies to deepen your understanding of the subject.