Medicine and Health
Identification of four biotypes in temporal lobe epilepsy via machine learning on brain images
Y. Jiang, W. Li, et al.
The study addresses the need to redefine neurological disease subtypes based on shared pathobiology to enable stratified, precision treatment. Temporal lobe epilepsy (TLE) exhibits clinical and imaging heterogeneity, and up to 40–50% of patients do not achieve long-term seizure freedom after anterior temporal lobectomy, suggesting distinct biological subtypes. Progressive gray matter atrophy—especially hippocampal atrophy and cortical thinning—has been linked to seizure burden and illness duration. However, spatiotemporal patterns of pathology have been difficult to characterize due to limited longitudinal data. The Subtype and Stage Inference (SuStain) algorithm can infer disease progression trajectories from cross-sectional data and has revealed distinct progressions in Alzheimer’s disease, schizophrenia, and frontotemporal dementia. The study’s purpose is to apply SuStain to T1-weighted MRI to uncover distinct atrophy trajectories in TLE, define biotypes, and evaluate their clinical and prognostic relevance, including differential outcomes to medication versus surgery and the feasibility of subtype-specific prognostic classifiers.
Prior work indicates that in TLE, hippocampal atrophy progresses faster with higher seizure frequency and cortical thinning progresses with longer disease duration. Event-based and progression modeling studies suggest sequences of atrophy can be inferred from cross-sectional imaging. AI and unsupervised learning have successfully stratified brain disorders into biologically meaningful subtypes. SuStain has identified multiple progression patterns in neurodegenerative and psychiatric diseases, including tau deposition trajectories in Alzheimer’s disease and gray matter atrophy trajectories in schizophrenia. Clinical literature shows that hippocampal sclerosis (HS) is associated with younger onset and poorer medication response, while absence of hippocampal atrophy can predict worse surgical outcomes; amygdala enlargement has been proposed as a separate TLE subtype with better response to antiepileptic drugs. These findings motivate imaging-based subtyping to capture heterogeneity and guide treatment decisions in TLE.
Design and cohorts: A discovery cohort included 296 individuals with TLE (139 females; age 27.2±8.7 years) and 81–91 healthy controls (39 females; age 26.4±6.7 years) recruited at West China Hospital (2014–2022). Inclusion: ILAE-diagnosed TLE; normal MRI or unilateral HS concordant with EEG; no bilateral HS or other extrahippocampal lesion. Exclusion: other neurological/psychiatric/systemic disease; substance abuse; other structural lesions except HS (per ILAE) confirmed by postoperative histopathology. A validation cohort included 109 TLE patients from three hospitals (Zhejiang University hospitals and Hainan Medical University). The study was registered (ChiCTR2200062562) and approved by ethics committee; informed consent obtained. Follow-up and outcomes: Patients were followed every 3 months until April 2023; final treatment categorized as operative group (OG; anterior temporal lobe surgery; n=152) or medication group (MG; n=144), based on medical advice and patient preference. Surgical effectiveness: seizure freedom at follow-up per ILAE criteria. Medication effectiveness: seizure freedom for ≥3× pre-treatment longest interseizure interval or ≥12 months. Imaging acquisition and processing: High-resolution T1-weighted MRI at 3 T (Siemens Trio; TR 1900 ms, TE 2.26 ms, flip angle 9°, 1 mm isotropic). FreeSurfer v6.0 used for segmentation. Subcortical gray matter volumes for 12 ROIs (bilateral hippocampus, amygdala, caudate, accumbens, pallidum, putamen, thalamus) and cortical thickness for 64 DK atlas regions were extracted. ROI measures were adjusted for sex, age, age², and total intracranial volume (TIV), then converted to z-scores relative to healthy controls and multiplied by −1 so larger z indicates more atrophy. SuStain modeling: Input was an M×N z-score matrix (M=296; N=23 ROIs selected a priori from ENIGMA-epilepsy literature showing reductions in mesial TLE). Waypoints used z thresholds 1, 2, 3. SuStain was run with 25 starting points and 1,000,000 MCMC iterations. Models with k=2–6 trajectories were compared using CVIC and out-of-sample log-likelihood; k=3 was optimal. SuStain provides, per individual, probabilities over trajectories, a most likely trajectory assignment, and a stage; subjects without deviations (all ROIs z<1) were assigned stage=0. Visualization and statistics: Stage-wise mean z-maps were visualized using ENIGMA toolbox. Spearman correlations tested association between SuStain stage and average cortical thickness and hippocampal volumes. Subtype signatures were derived by averaging ROI z-scores and comparing to controls and between subtypes (two-sample t-tests, FDR correction). Reproducibility and stability: Validation cohort re-estimated trajectories; subtype-specific z-maps compared between discovery and validation (Pearson r with spin test). Stability assessed by feature-reduction (23→13 ROIs) and ten-fold cross-validation generalization (consistency of subtype labels; correlation of stages). Clinical comparisons: One-versus-all and one-versus-one analyses of demographics, TIV, seizure lateralization, MRI HS rate, histories (febrile seizures, encephalitis/meningitis), aura, seizure frequency/type, medications, EEG pathology laterality, treatments, and outcomes (ANOVA with LSD for continuous; chi-square for categorical; FDR correction). HS included as covariate in sensitivity analyses. Prognosis prediction: For 145 postsurgical follow-up patients, SVM classifiers with ten-fold CV predicted OG+ vs OG−. Features: baseline clinical, MRI, or both; PCA retained PCs explaining >95% variance; kernels tested: linear/RBF/polynomial. Performance evaluated by accuracy, sensitivity, specificity, Youden index; permutation tests assessed significance. A subtype-based framework trained separate SVM sub-classifiers per SuStain subtype and compared with a subtype-agnostic classifier.
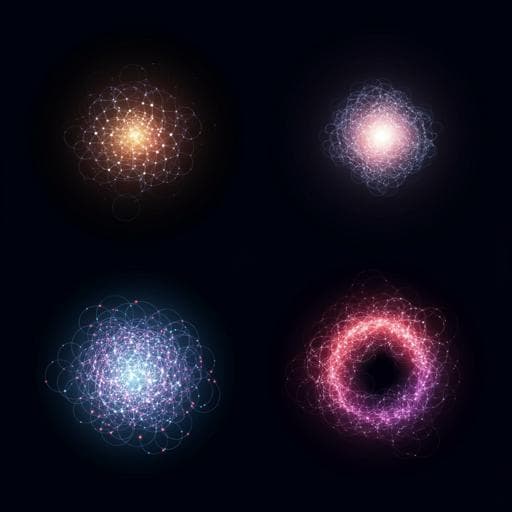
- Three distinct atrophy trajectories identified by SuStain from cross-sectional MRI of 296 TLE patients: (1) left hippocampus → left thalamus → right thalamus → left entorhinal/cortex; (2) right hippocampus → right thalamus → left thalamus → left hippocampus → cortex; (3) cortex-predominant starting in bilateral frontal regions, then spreading to parietal/occipital/temporal cortices, finally involving hippocampus and thalamus. Patterns were similar in short-duration and long-duration subsamples. - SuStain stage correlated with atrophy severity: average cortical thickness (trajectory 1 r=0.599, p<0.001; trajectory 2 r=0.791, p<0.001; trajectory 3 r=0.847, p<0.001), left hippocampal volume (trajectory 1 r=0.627, p<0.001; trajectory 2 r=0.577, p<0.001; trajectory 3 r=0.431, p=0.005). Right hippocampal volume correlation was significant only in trajectory 1 (r=0.269, p=0.013). - Four neuroanatomical subtypes (signatures): subtype 1 left hippocampus-predominant; subtype 2 right hippocampus-predominant; subtype 3 cortex-predominant; subtype 4 “normal” signature with amygdala enlargement. Subtype proportions: 28.7%, 38.2%, 13.9%, and 19.2%, respectively. Subtype 4 had significantly larger bilateral amygdala than other subtypes and controls (t>6.39, p<1e-6). - Reproducibility: Validation cohort (n=109) replicated three trajectories initiating in left hippocampus, right hippocampus, and cortex. Subtype-specific z-maps were highly consistent between discovery and validation (r>0.7, p<1e-9). Stability/generalization: 93.9% label consistency with fewer features; ten-fold CV showed 98.6% consistency of subtype assignments; stages correlated strongly with original model (Spearman r=0.986, p<0.001). Longitudinal subsample (n=23; ~39 months) showed stable subtype labels over time. - Clinical differences among subtypes: HS on MRI was far more common in subtypes 1 and 2 (95.3% and 92.9%) than subtypes 3 (39.0%) and 4 (42.1%). Seizure lateralization matched hippocampal-predominant side in subtypes 1 and 2. Subtype 1 had youngest onset (12.3±7.7 years; t=-4.34, p<0.0001). Hippocampal-predominant subtypes had longer illness duration than subtypes 3 and 4 (t=3.70, p=0.0003). Subtype 3 had larger TIV than others. After controlling for HS, subtype remained associated with age of onset (t=-3.51, p=0.001), illness duration (t=-3.15, p=0.002), and medication outcomes (χ²=5.64, p=0.018). - Treatment outcomes differ by subtype: Medication group (n=107 followed): seizure-free rate higher in subtype 4 (39.29%) vs others (12.66%) (χ²=9.29, p=0.0023). Surgery group (n=145 followed): seizure-free rate lower in subtype 4 (45.00%) vs others (69.60%) (χ²=4.66, p=0.031). HS+ patients had younger onset than HS− (t=-3.49, p=0.001) and better surgical outcomes than HS− (χ²=5.99, p=0.014). - Prognosis prediction: Subtype-based SVM framework (separate sub-classifiers per subtype) achieved overall accuracy 71.72%, specificity 81.03%, sensitivity 47.87% (Youden index J=0.289), significantly above permutation (p=0.012). A subtype-agnostic clinical-features-only model had 67.59% accuracy, 89.58% specificity, 24.49% sensitivity, and non-significant J=0.141 (p=0.307). Adding MRI features without subtype information did not improve performance (J=0.130; accuracy 66.90%; sensitivity 24.49%; specificity 88.54%).
Applying SuStain revealed heterogeneous spatiotemporal atrophy progressions in TLE, supporting biologically distinct biotypes. Two trajectories highlight hippocampal-first degeneration with propagation to ipsilateral and contralateral thalamus and cortex, consistent with known corticothalamic involvement in seizure propagation. A cortex-first trajectory suggests delayed hippocampal involvement and heterogeneity in cortical versus mesial temporal neurodegeneration. SuStain stages correlated with atrophy severity, indicating that cross-sectional trajectories reflect underlying pathophysiological progression. The four derived subtypes showed distinct clinical profiles and treatment responses: hippocampal-predominant subtypes (high HS rates, ipsilateral seizure focus) had favorable surgical outcomes, while the “normal” signature with amygdala enlargement had better medication response but poorer postsurgical seizure freedom, aligning with prior descriptions of TLE with amygdala enlargement. Subtype-informed prognostic modeling improved identification of surgical non-responders compared with clinical data alone, underscoring the value of imaging-based taxonomy for stratification and prognosis. Findings align with recent progression-modeling studies in epilepsy, reinforcing hippocampal-dominated trajectories as a key feature in TLE and supporting personalized management strategies based on biotype.
The study identifies three distinct atrophy trajectories and four MRI-derived biotypes in TLE, each with characteristic neuroanatomical patterns, clinical features, and differential long-term outcomes to medication and surgery. SuStain-derived stages reflect atrophy severity, and subtypes are reproducible, stable, and generalizable. Subtype-based classifiers significantly improve prediction of surgical outcomes over clinical information alone, demonstrating translational potential for precision neurology. Future work should validate trajectories with longitudinal onset-to-outcome imaging, investigate mechanistic bases (connectomics, cytoarchitecture, metabolism, neurotransmitter systems, gene expression, cognition), refine subtype granularity, and model treatment-response trajectories across SuStain stages in larger multicenter cohorts.
- Trajectories were inferred from cross-sectional MRI; longitudinal imaging, particularly at epilepsy onset, is needed to confirm true temporal progression and disentangle progression from initial injury. - Single-scanner/protocol processing improves consistency but limits generalizability; larger, multicenter longitudinal samples would strengthen validation. - Sample-to-feature ratio was relatively low, potentially underpowering some analyses, although stability was verified at reduced spatial resolution. - Mechanistic underpinnings of subtypes (connectivity, cytoarchitecture, metabolism, receptor systems, gene expression, cognitive function) remain unresolved. - Insufficient sample size to characterize how treatment response varies with SuStain stage within each subtype. - While a four-subtype solution captured heterogeneity here, more subtle subtypes may exist and warrant exploration.
Related Publications
Explore these studies to deepen your understanding of the subject.