Medicine and Health
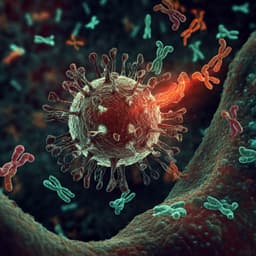
Humoral and cellular immune responses to COVID-19 mRNA vaccines in immunosuppressed liver transplant recipients
T. Nogimori, Y. Nagatsuka, et al.
This critical study led by Takuto Nogimori and his team investigates the immune response to COVID-19 vaccines in liver transplant recipients. Results reveal that despite weaker antibody responses, a third vaccination significantly enhances immune response, highlighting the importance of further research to maximize CD8+ T-cell efficacy.
Related Publications
Explore these studies to deepen your understanding of the subject.