Medicine and Health
High Prevalence of Respiratory Co-Infections and Risk Factors in COVID-19 Patients at Hospital Admission During an Epidemic Peak in China
X. Zhu, F. Tian, et al.
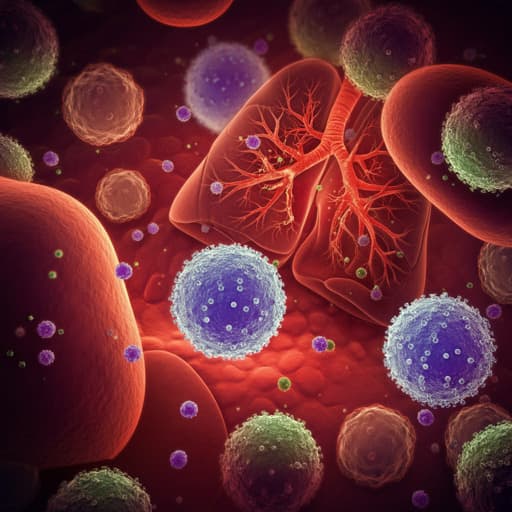
The study addresses how frequently and which types of respiratory co-infections occur in hospitalized COVID-19 patients during an epidemic peak in China following relaxation of public health measures (December 2022), and which clinical factors predict mortality. Context: Co-infections with bacterial and viral respiratory pathogens can exacerbate disease severity and increase mortality in COVID-19. Reported co-infection rates vary widely across regions and methods, with bacteria such as Streptococcus pneumoniae, Klebsiella pneumoniae, Staphylococcus aureus, and Haemophilus influenzae, and viruses such as influenza A/B and RSV commonly implicated. The post-policy-shift surge in China created a need to quantify co-infection prevalence, evaluate antibiotic use, and identify risk indicators to inform clinical management. Purpose: To determine prevalence and patterns of respiratory co-infections, assess antibiotic utilization, and analyze risk factors for death among hospitalized COVID-19 patients during the epidemic peak in Guangxi, China.
The authors summarize prior evidence that co-infections are common in COVID-19 and can exceed 50% among deceased patients. Bacterial co-pathogens frequently include K. pneumoniae, S. pneumoniae, S. aureus, and H. influenzae; viral co-pathogens include influenza A/B and RSV. Antibiotic misuse during COVID-19 may fuel antimicrobial resistance and disrupt gut microbiota, potentially worsening outcomes. Prior studies report heterogeneous co-infection rates due to differences in patient populations, detection methods (culture vs PCR), and pathogen panels; some cohorts in China reported very high rates with broad detection panels. Vaccination against pathogens like pneumococcus, Hib, and influenza may mitigate co-infection risk and severity. The literature also links elevated inflammatory markers (e.g., CRP, D-dimer) with bacterial co-infections and adverse cardiac outcomes. Evidence on viral–viral interactions (e.g., FluA enhancing or inhibiting SARS-CoV-2 infection) is mixed, highlighting the complexity of co-infections.
Design and setting: Retrospective cohort study at the Affiliated Hospital of Youjiang Medical University for Nationalities, Guangxi, China. Period: December 14, 2022 to January 30, 2023. Participants: 716 hospitalized patients diagnosed with COVID-19 according to the Diagnosis and Treatment Plan for SARS-CoV-2 Infection (10th Edition). Data collected: demographics, vaccination status, comorbidities, clinical manifestations, laboratory data at admission, treatments (including antivirals, respiratory support, antibiotics), clinical classification (mild, moderate, severe, critical), ICU admission, outcomes (length of stay, death). Ethics: Approved by the hospital ethics committee (YYFY-LL-2023-119); de-identified retrospective data, consent waived. Specimen collection and laboratory testing: Throat swabs collected at admission. SARS-CoV-2 detected using DaAnGene PCR kit (DA0933). Twelve respiratory pathogens detected via qPCR using Sansure Multiplex kits (S3310E and S3066E). Pathogens: six bacteria (Klebsiella pneumoniae, Legionella pneumophila, Streptococcus pneumoniae, Haemophilus influenzae type b, Pseudomonas aeruginosa, Staphylococcus aureus), five viruses (influenza A, influenza B, respiratory syncytial virus, adenovirus, human rhinovirus), and Mycoplasma pneumoniae. Clinical management context: Antiviral therapy per national guideline (10th Edition): options included nirmatrelvir/ritonavir, remdesivir, monoclonal antibodies; supportive care per severity. Severity definitions: moderate (fever >3 days with cough/SOB; RR <30; SpO2 >93%), severe (RR >30, SpO2 <93%, progressive lesions), critical (respiratory failure, shock, or organ dysfunction). Discharge criteria included stable vitals and improved pulmonary lesions. Statistical analysis: Categorical variables as n (%); continuous variables as medians (IQR). Group comparisons via Wilcoxon rank-sum, Pearson’s chi-squared, Fisher’s exact tests. Associations among categorical variables via chi-square and Cramer’s V. Co-infection intersections visualized with UpSetR (v1.4.0). Risk factor analysis via univariable and multivariable Cox proportional hazards regression using R packages StepReg (v1.4.4) and survival (v3.5.0), forward stepwise selection. Kaplan–Meier survival and log-rank tests presented for key factors.
- Cohort characteristics (n=716): 61% male; median age 64 years (IQR 49–73); 92% vaccinated. Clinical severity: moderate 85% (611), severe 11% (78), critical 3.8% (27). Mortality 6.3% (45). Median hospital stay 7 days (IQR 5–9).
- Co-infection prevalence: 76.82% (550/716) had ≥1 respiratory co-pathogen detected by qPCR; significant differences in length of stay and leukocyte counts between co-infected vs non–co-infected groups (e.g., LOS 7 vs 8 days; p=0.003). Any bacterial co-infection: 74% (529/716). Any viral co-infection: 15% (108/716). Concurrent bacteria+virus: 12% (87/716). Mp detected in 0.56% (4/716). No Legionella pneumophila detected.
- Pathogen-specific detection rates among all patients: Streptococcus pneumoniae 62.01% (444), Haemophilus influenzae type b 19.97% (143), Klebsiella pneumoniae 11.45% (82), Pseudomonas aeruginosa 10.20% (73), influenza A 5.87% (42), RSV 5.59% (40), adenovirus 3.77% (27), Staphylococcus aureus 3.63% (26), influenza B 1.82% (13), Mycoplasma pneumoniae 0.56% (4), human rhinovirus 0.14% (1).
- Co-infection patterns: Single pathogen in 42.46% (304/716), most commonly S. pneumoniae (220, 30.73%). Common combinations: S. pneumoniae + Hib (59, 8.24%), S. pneumoniae + FluA (25, 3.49%), S. pneumoniae + K. pneumoniae (22, 3.07%); triple: S. pneumoniae + Hib + K. pneumoniae (19, 2.65%), S. pneumoniae + Hib + P. aeruginosa (9, 1.26%). One case had eight pathogens detected.
- Severity associations (Table 3): S. pneumoniae detection higher in moderate vs severe/critical (p<0.001); RSV higher in severe (p=0.041); P. aeruginosa higher in critical (30%; p=0.008). FluB, Mp, HRV detected only in moderate cases.
- Age-related findings: All 12 pathogens detected in 0–1 year group; 11 (except Mp) in ≥65 years. S. pneumoniae positivity near 50% (11/23) in 1–12 years; S. aureus and FluA rates higher in <18 years.
- Antibiotic use: 65.5% (469/716) received antibiotics. Among pathogen-positive (n=550), 64.9% (357) received antibiotics. Notably, antibiotics were used in 52.4% of cases with only viral co-infection and 67.5% with no pathogen detected, indicating possible irrational use. Antibiotics usage associated with hypoproteinemia and lymphopenia, but not with death.
- Risk factors for death (Cox regression, n=670): • Dyspnea: adjusted HR 2.09 (95% CI 1.11–3.95; p=0.023). • Hypoproteinemia: adjusted HR 1.95 (1.03–3.66; p=0.039). • Low lymphocyte count (<0.8×10^9/L): adjusted HR 1.99 (1.06–3.75; p=0.032). High lymphocyte count (>4×10^9/L) not significantly different vs normal. • Mycoplasma pneumoniae co-infection: adjusted HR 26.03 (3.29–206.06; p<0.01), despite low prevalence (4 cases).
- Correlations (Table 5): Lymphopenia associated with H. influenzae co-infection (p=0.024; Cramer’s V=0.102). Hypoproteinemia associated with S. pneumoniae (p=0.011; V=0.099), H. influenzae (p=0.031; V=0.085), and P. aeruginosa (p=0.044; V=0.081). CRP associated with S. pneumoniae (p=0.007; V=0.107) and P. aeruginosa (p=0.017; V=0.097). No significant association between antibiotic use and mortality.
The study demonstrates a very high prevalence of respiratory co-infections among hospitalized COVID-19 patients during the epidemic peak following policy relaxation in China. Broad qPCR-based screening likely increased detection compared with culture-based approaches and, along with high inpatient density and moderate-to-severe case mix, contributed to the high rates. The predominance of S. pneumoniae, Hib, and K. pneumoniae aligns with known colonizers that can cause secondary lower respiratory infections in immunocompromised hosts. Viral co-infections (notably influenza A and RSV) were also common and clinically relevant. The findings underscore the importance of comprehensive diagnostic evaluation for co-infections to guide therapy. Despite frequent bacterial detections, antibiotic prescribing did not always match pathogen evidence, highlighting opportunities for antibiotic stewardship to minimize unnecessary exposure and resistance risks. The identification of dyspnea, hypoproteinemia, and lymphopenia as independent mortality risk factors emphasizes prioritizing respiratory support and nutritional optimization, while the strong association of M. pneumoniae co-infection with mortality suggests vigilance for and prompt treatment of atypical bacterial co-infection. Correlations between co-infections and inflammatory markers (CRP) support their utility in risk stratification. Vaccination strategies against pneumococcus, Hib, and influenza may reduce co-infection burden and improve outcomes during COVID-19 surges.
In a cohort of 716 hospitalized COVID-19 patients during an epidemic peak in China, 76.82% had at least one respiratory co-pathogen detected by qPCR, with frequent bacterial (especially S. pneumoniae, Hib, K. pneumoniae) and notable viral (FluA, RSV, adenovirus) co-infections. Antibiotic use was common but sometimes discordant with microbiologic findings, indicating room for stewardship improvements. Dyspnea, hypoproteinemia, lymphopenia, and M. pneumoniae co-infection independently predicted higher mortality. Clinical management should include robust diagnostic testing for co-infections, targeted antibiotic use, respiratory support, and nutritional optimization. Broader vaccination against pneumococcus, Hib, and influenza may help prevent co-infections and reduce adverse outcomes. Future research should incorporate broader pathogen panels (including fungi), control groups, vaccination histories, and methods to distinguish community- vs hospital-acquired infections to refine clinical relevance and therapeutic strategies.
- Pathogen detection limited to the 12 targets on the multiplex PCR panel; potential co-infections (e.g., fungal) not assessed.
- qPCR positivity indicates presence of pathogen nucleic acid but does not confirm active infection; results may reflect colonization.
- Unable to distinguish community-acquired from nosocomial bacterial infections.
- Lack of data on pneumococcal, Hib, and influenza vaccination status precluded analyses of vaccine impact on co-infections.
- No healthy or mildly affected COVID-19 control groups, limiting assessment of clinical relevance of PCR detections.
- Some detected pathogens may relate to preexisting chronic conditions or healthcare exposure; attribution of infection source is uncertain.
Related Publications
Explore these studies to deepen your understanding of the subject.