Medicine and Health
Gut microbiota dysbiosis is associated with altered tryptophan metabolism and dysregulated inflammatory response in COVID-19
M. Essex, B. M. Pascual-leone, et al.
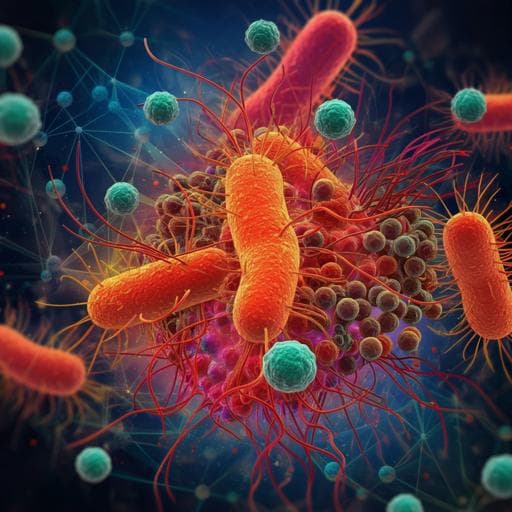
COVID-19, caused by SARS-CoV-2, exhibits heterogeneous clinical outcomes where a subset of patients progress to severe pneumonia, ARDS, coagulopathy, and multiorgan failure. Evidence suggests severity is driven by dysregulated immune responses with elevated proinflammatory cytokines (e.g., IL-6, TNFα, IFNγ), T cell lymphopenia, and myeloid alterations. Known risk factors (age, sex, comorbidities, genetics, IFN autoantibodies) do not fully explain outcome variability. The human respiratory and gut mucosa harbor diverse microbiota producing metabolites (SCFAs, tryptophan catabolites, secondary bile acids) that shape immunity. Prior studies linked COVID-19 with reduced bacterial diversity, enrichment of opportunists, decreased commensals in the upper airway, and elevated inflammatory cytokines. This study investigates how microbiome composition and function, host metabolome (especially tryptophan and bile acid pathways), and immune responses interrelate with COVID-19 status and severity, using repeated sampling and integrated multi-omics with post-hoc confounder analysis.
Background work shows: (1) severe COVID-19 is associated with heightened proinflammatory cytokines and innate immune dysregulation; (2) intraindividual microbiota differences correlate with peripheral cytokine production capacities; (3) COVID-19 has been associated with reduced gut diversity, enrichment of opportunistic pathogens, and depletion of upper airway commensals; (4) microbial metabolites (tryptophan catabolites, SCFAs, secondary bile acids) modulate host immunity via receptors such as AHR, PXR, TGR5, and FXR. These findings motivated testing links among dysbiosis, metabolite shifts, and inflammatory responses in COVID-19.
Study design: Prospective observational cohort (Pa-COVID-19, Charité–Universitätsmedizin Berlin) of hospitalized, PCR-confirmed COVID-19 patients enrolled March–June 2020 (pre-vaccination and pre-VOCs) and age/sex-matched uninfected controls. Ethical approvals EAZ/206/20 and EA2/068/20; informed consent obtained. Disease severity classified by WHO OSCI: mild (1–4) vs severe (5–8). Cohort and sampling: 30 hospitalized COVID-19 patients (22 mild, 8 severe; 3 in-hospital deaths) and 15 uninfected controls. Median hospitalization 8 days (range 3–32; excluding deaths). Samples collected longitudinally: oropharyngeal (OP) swabs (n=94 total; 75 post-QC), tracheobronchial secretions (TBS; n=18; low reads, most excluded), stool (n=81; 72 post-QC), plasma (n=96), urine (n=27). PBMCs obtained from 14 COVID-19 patients (early phase) and 11 controls; T and B cells depleted to enrich myeloid compartment. Severe cases and those requiring ICU/MV were further stratified into early (≤10 days since onset) and late (>10 days) observation phases. Assays: (1) Shotgun metagenomic sequencing of stool, OP, and TBS (Illumina NovaSeq; average depth ~56 Gb); taxonomic profiling with mOTUs; diversity analyses (alpha: Shannon; beta: PCoA). (2) Plasma and urine metabolomics: Biocrates MxP Quant 500 targeted panel; dedicated LC-MS methods for tryptophan derivatives; GC-MS for central carbon metabolites; rigorous QC (SST, internal standards, pooled QC, batch correction). (3) Plasma cytokines by multiplex bead-based ELISA/cytometric bead array (e.g., IFNs, TNFα, IP-10/CXCL10, CCL2, IL-10, IL-1 family). (4) PBMC single-cell RNA-seq (10x Genomics, TotalSeq hashing); preprocessing with Cell Ranger; QC (mitochondrial read %, UMI/gene thresholds); normalization (TP10K, log-transform), PCA/UMAP, Louvain clustering, cell-type annotation via marker genes. (5) Upper airway IFN gene expression by RT-qPCR (normalized to GAPDH). (6) Viral load quantification by RT-PCR (cobas 6800/8800) with calibrated standards. Statistics: All analyses in R with targets workflow. Step 1: association screening between -omics features and clinical variables using standardized non-parametric effect sizes (Cliff’s delta for binary, Spearman’s ρ for continuous) with BH FDR correction. Step 2: post-hoc confounder analysis via iterative nested regression and likelihood ratio tests in linear mixed-effects models (random intercept for patientID) comparing models with and without candidate confounders (e.g., antibiotics, hospitalization duration, HAP, bacteremia/sepsis, comorbidities). Features classified as robust (not confounded), confirmed, or not significant (FDR-adjusted). Cross-omics integration: robust severity-associated features from one modality included as covariates when testing others (e.g., testing whether kynurenine statistically constrains IFNγ-severity association).
- Microbiota: Gut microbiota alpha diversity was significantly decreased in COVID-19 vs controls (Kruskal–Wallis P < 0.001). Beta diversity reflected disease status, severity, and antibiotic intake. Mild cases showed lower abundances of Lachnospiraceae, Clostridiaceae, Faecalibacterium spp., and Eggerthellaceae relative to controls; severe cases had decreased Intestinimonas, Eubacteriaceae, and Tuerkeria vs mild. Antibiotics associated with depletion of Firmicutes, Romboutsia, Coprococcus, Roseburia and enrichment of Enterococcus and Lactobacillus. Hungatella abundance correlated with comorbidities (mild) and HAP (severe). Oropharyngeal microbiota composition was primarily associated with antibiotic intake; alpha diversity was lower in COVID-19 than controls, with highest variability in severe cases; Prevotella and Slackia correlated with HAP.
- Immune response: Plasma showed increased proinflammatory cytokines in COVID-19 vs controls (e.g., TNFα, IP-10/CXCL10, CCL2, IL-10, IL-1 family); IFNs were elevated early and decreased later, while inflammatory cytokines remained high in severe disease. scRNA-seq of PBMCs (innate-enriched) revealed increased classical monocytes in severe COVID-19, depletion of non-classical monocytes and conventional dendritic cells in early infection, and NK cell depletion in severe cases. ISGs were enriched and correlated with circulating type I/II IFNs; airway IFN gene expression increased in mild cases.
- Metabolome: Severe COVID-19 associated with marked perturbation of tryptophan metabolism. Lower plasma levels of dietary tryptophan (ρ = −0.68, FDR < 0.0001), 5-hydroxytryptophan (ρ = −0.38, FDR = 0.0003), and microbial indole metabolites (tryptamine, indole-3-propionic acid, indole-3-acetic acid), alongside increased kynurenine. Reduced lysophosphatidylcholines and secondary bile acids observed in severe disease. Several metabolite shifts associated with severity persisted after post-hoc confounder analysis (e.g., hospitalization, antibiotics, comorbidities).
- Cross-omics links: Reduced tryptophan metabolites correlated with depletion of Faecalibacterium; reduced indole-3-propionic acid also related to Faecalibacterium depletion. Decreased tryptophan and increased kynurenine (reflecting IDO1 activity) linked to elevated proinflammatory cytokines (e.g., IFNγ). Authors hypothesize altered liganding of AHR/PXR by tryptophan catabolites contributes to immune dysregulation. Secondary bile acid decreases suggest impaired microbiota-derived bile acid signaling (TGR5/FXR) with potential immune consequences.
- Cohort and data scope: 30 COVID-19 patients (22 mild, 8 severe; 3 deaths) and 15 controls; 96 plasma and 27 urine metabolomics samples; 75 OP and 72 stool metagenomes post-QC; PBMC scRNA-seq from 14 patients and 11 controls.
The study supports the hypothesis that COVID-19 severity is linked to coordinated disturbances in gut microbiota, host–microbe co-metabolism, and systemic immune responses. Gut dysbiosis with depletion of beneficial commensals (notably Faecalibacterium and other Clostridiales) is associated with reduced microbial indole-derived tryptophan catabolites and lower host tryptophan/serotonin pathway intermediates, alongside increased kynurenine. These shifts likely alter signaling through AHR and PXR, potentially stabilizing proinflammatory cytokine production and contributing to T cell dysfunction in severe disease. Reduced secondary bile acids and lysophosphatidylcholines further indicate disrupted lipid and bile acid signaling that can modulate innate and endothelial responses. While antibiotic exposure and hospitalization influence the oropharyngeal and some gut taxa, many microbiome–metabolome–immune associations remained robust after post-hoc confounder analysis. Cross-omics modeling suggests that metabolite changes (e.g., kynurenine) can partially constrain cytokine–severity associations, supporting a mechanistic link between metabolic reprogramming and inflammatory dysregulation during severe COVID-19.
This multi-omics study identifies coordinated alterations of the gut microbiome, tryptophan and bile acid metabolism, and systemic inflammatory responses associated with COVID-19 severity. Depletion of beneficial commensals and reduced microbial/host tryptophan metabolites, together with increased kynurenine, correlate with heightened proinflammatory cytokines, implicating microbiome–metabolite–immune axes (e.g., AHR/PXR signaling) in severe disease pathogenesis. Findings generate testable hypotheses for targeted modulation of microbiota-derived metabolites and pathways to restore immune homeostasis. Future work should validate these associations in larger, multi-center cohorts, include non-COVID ICU controls, incorporate dietary/nutritional data, analyze lung-local immune responses, and employ mechanistic in vitro and animal models to dissect causal roles of specific tryptophan catabolites and secondary bile acids across disease phases.
- Single-center study with modest sample size limits generalizability; requires validation in larger cohorts.
- Lack of very-early infection samples precludes conclusions about earliest mechanistic events.
- No detailed dietary or in-hospital nutrition data, which may affect microbiota and metabolites.
- Absence of an ICU/non-COVID critical illness control group hinders disentangling COVID-19-specific vs hospitalization/critical care effects.
- Limited analysis of lung immune responses; many respiratory microbiome samples (TBS/OP) had insufficient reads.
- Potential confounding from antibiotics and hospitalization factors remains despite post-hoc adjustments.
Related Publications
Explore these studies to deepen your understanding of the subject.