Medicine and Health
Gut-derived short-chain fatty acids modulate skin barrier integrity by promoting keratinocyte metabolism and differentiation
A. Trompette, J. Pernot, et al.
The study addresses how gut-derived short-chain fatty acids (SCFA), particularly butyrate, influence skin barrier integrity and the development of atopic dermatitis (AD). With rising global prevalence of allergic and autoimmune diseases linked to westernized lifestyle, barrier dysfunction is hypothesized to permit allergen ingress, leading to sensitization and the atopic march. AD commonly begins in early life and is associated with subsequent allergic diseases. Keratinocyte differentiation and lipid/protein production establish the stratum corneum, the cornerstone of barrier function. Epidemiological evidence indicates reduced SCFA-producing gut microbiota and lower SCFA levels in infants and children with AD or at risk of allergic sensitization. The research tests whether dietary fiber and SCFA can strengthen the epidermal barrier to limit percutaneous allergen penetration, systemic sensitization, and AD-like skin inflammation (ADLSI), and explores cellular mechanisms in keratinocytes.
Prior work shows dietary fiber fermentation by gut microbiota generates SCFA that modulate immune responses locally and at distal sites, with known roles for SCFA as HDAC inhibitors, GPCR ligands (FFAR2/FFAR3), and metabolic substrates. SCFA effects on non-immune structural cells (e.g., epithelial barriers) are less characterized beyond the gut. Epidemiological and microbiome studies report reduced fecal SCFA (notably butyrate) and diminished butyrate-producing taxa in infants/children with AD or those who later develop allergic sensitization. Skin barrier integrity depends on keratinocyte-produced proteins (e.g., loricrin, filaggrin) and lipids (ceramides, cholesterol); Th2 cytokines can impair these pathways. These findings motivated testing the gut–skin axis and SCFA in skin barrier regulation and AD pathogenesis.
- Animals and diets: Female BALB/c mice were housed SPF. Mice received either a low-fibre diet supplemented with 30% inulin (high-fibre diet, HFD) or 30% cellulose (control diet, CD) for 4 weeks before HDM exposure and throughout. For SCFA experiments, weanling mice on low-fibre diet received sodium acetate, propionate, or butyrate in drinking water (400 mM) for 2 weeks prior to and during sensitization.
- AD-like skin inflammation (ADLSI) model: Dorsal skin was shaved and occluded patches containing 15 µg of Dermatophagoides pteronyssinus HDM extract in 80 µL saline were applied twice weekly under bioclusive dressing for 1–2 weeks, with 2-day recovery periods. Controls included saline patches.
- Clinical and barrier assessments: Disease severity scored (presence of dryness, rash, excoriation, baldness, lichenification; 0/1 each). Transepidermal water loss (TEWL) measured by TEWAmeter. Histology (H&E) to assess epidermal thickening, immune infiltration, and stratum corneum (SC) thickness; loricrin IHC quantified.
- Allergen sensitization: Serum HDM-specific IgE quantified by ELISA at endpoint.
- Allergen ingress and APC function: FITC–dextran (10 kDa) applied topically with HDM to assess percutaneous penetration and uptake by dermal APCs via flow cytometry; FITC–dextran and DQ-ovalbumin given intradermally to bypass epidermis for uptake/processing capacity.
- Immune phenotyping: Flow cytometry of skin single-cell suspensions characterized APC subsets (cDC2, LCs, monocyte-derived DCs, macrophages), PD-L2 expression, γδ T cells (activation via CD44), ILCs (IL-4, IL-5, IL-17A), CD4+ T cells (frequency, CD44 activation, cytokine production), and Foxp3+ Tregs; analyses at 1 week (pre-symptomatic) and after 2 weeks sensitization. Baseline (naïve) immune composition assessed.
- Keratinocyte analyses in vivo: Flow cytometric quantification of epidermal keratinocytes (CD326+), hair bulge CD34+ cells, differentiation status via CD49f (CD49f+ undifferentiated vs CD49f− differentiating/differentiated). FACS-purified keratinocytes analyzed by qRT-PCR for barrier proteins (Ivl, Lor, Flg, Lce1m, Clsp) and lipid enzymes (Acc, Elovl6, Cers3, Smpd1, B3Galt2). Mitochondrial mass and membrane potential assessed by MitoTracker dyes.
- Transcriptomics: RNA-seq on lesional skin from control vs butyrate-treated animals; differential expression via Voom/Limma (FDR < 0.1, FC > 2) and GO enrichment (Gorilla). Selected genes validated by qRT-PCR.
- Lipidomics and metabolomics: Skin lipidomics to quantify cholesterol (UHPSFC/ESI-QTOF-MS) and ceramide classes including ester-linked omega-hydroxy (EO) ceramides (UPLC/ESI-MS/MS). Total LCFA/VLCFA profiled (GC-FID). Multiple pathway targeted metabolomics on FACS-isolated murine keratinocytes (HILIC-MS/MS; pathway enrichment by MetaboAnalyst).
- Butyrate biodistribution and tracing: Oral 13C-butyrate gavage; 13C detection in skin by HILIC-HRMS at 45 min. In vitro HEK treated with 13C-butyrate; isotopologue incorporation into TCA intermediates measured by HILIC-HRMS.
- Human epidermal keratinocyte (HEK) in vitro model: Primary HEK cultured and treated with 500 µM butyrate for 24–96 h. Controls included vehicle and 500 µM valproate (HDAC inhibitor control). Calcium (1.2 mM) used for positive control differentiation. Outcomes: phase-contrast morphology, TEM ultrastructure, total RNA/protein content, qRT-PCR for differentiation markers (DSG1, KRT1, KRT10, IVL, FLG, CLSP), ACC/ELOVL4/SLC27A1/SLC27A2 expression, flow cytometry for size (FSC), granularity (SSC), lysosomes (LysoTracker), mitochondrial mass (MitoTracker Green), MMP (JC-1), LCFA uptake (BODIPY FL C16). Ceramide production (NS, NDS) quantified by UPLC/ESI-MS/MS.
- Metabolic functional assays: Seahorse XF Mito Stress Test for OCR (basal and maximal respiratory capacity) and Glycolysis Stress Test (ECAR). FAO activity measured colorimetrically. Pharmacologic FAO inhibition with etomoxir (20 µM) assessed effects on HEK differentiation phenotype.
- Statistics: Student’s t-test or Mann-Whitney where appropriate; mean ± SEM; significance P < 0.05; sample sizes per figure legends.
- Dietary fiber and SCFA reduce AD-like disease: Mice on high-fiber diet (inulin) had lower clinical scores and TEWL versus cellulose controls, with reduced epidermal thickening and immune cell infiltration. Oral SCFA supplementation on a low-fiber diet recapitulated protection, most pronounced with butyrate, which reduced disease severity, TEWL, epidermal thickness, and serum HDM-specific IgE. Orally delivered 13C-butyrate reached skin within 45 minutes.
- Transcriptomic and gene expression changes: 195 genes were differentially expressed in butyrate-treated lesional skin (FDR < 0.1, FC > 2). GO terms enriched included negative regulation of immune responses and keratinization/cornified envelope. qRT-PCR showed reduced pro-TH2 mediator IL-33 and IL-4Rα; reduced S100a8, Cxcl1 (TH17/TH22-associated), IL-20, and IL-1β. Itch-related Areg decreased; Sema3d increased. Barrier genes increased: Ivl, Lor, Flg, Lce1m, Clsp; lipid metabolism genes increased: Acc, Elovl6, Cers3, Smpd1, B3Galt2.
- Early immune responses blunted post-HDM with preserved APC composition: Frequencies of cDC2, LCs, monocyte-derived DCs, and dermal macrophages were similar, but PD-L2 expression and PD-L2+ APC frequencies decreased. γδ T cell activation (CD44) and ILC2 IL-4 production reduced; CD4+ T cells decreased in frequency and activation with diminished IL-4, IL-5, IL-17A production. Tregs were not increased (actually reduced). When HDM was injected intradermally to bypass the barrier, TH2 responses were no longer impaired, implicating barrier effects rather than direct immune modulation.
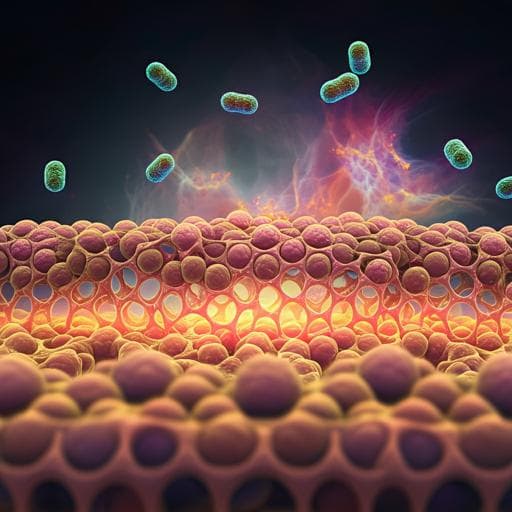
- Enhanced barrier function at baseline and after allergen exposure: Butyrate improved baseline barrier (lower TEWL) and tended to increase SC thickness before exposure; baseline keratinocytes had elevated barrier gene expression without changes in TH2 cytokines. After HDM, SC was significantly thicker, and loricrin formed a continuous layer in butyrate-treated skin but was reduced/disrupted in controls. Cholesterol and EO ceramides increased with butyrate; EO ceramides declined in controls after HDM but increased with butyrate. Topical FITC–dextran uptake by dermal APCs was reduced (less percutaneous ingress), while intradermal antigen uptake/processing was normal, indicating strengthened epidermal barrier rather than APC dysfunction.
- Keratinocyte differentiation promoted in vivo and in vitro: In mice, butyrate increased proportions of CD49f− differentiating/differentiated keratinocytes at baseline and post-HDM and elevated expression of Lce1m, Lor, Flg and lipid enzymes. In HEK, butyrate induced morphological and ultrastructural hallmarks of differentiation, reduced RNA/protein synthesis, increased early (DSG1, KRT1/10) and late (IVL, FLG, CLSP) differentiation markers, and increased ceramide (NS, NDS) production.
- Mechanism: metabolic reprogramming rather than HDAC inhibition. Valproate (HDACi) did not mimic butyrate’s effects on HEK morphology, RNA synthesis, differentiation markers, or organelle content; CDKN1A/B were not induced. Metabolomics of murine keratinocytes showed altered pathways linked to mitochondrial FAO and fatty acid synthesis. 13C-butyrate tracing demonstrated incorporation into TCA intermediates (e.g., citrate). Butyrate increased ACC and ELOVL4 expression and boosted LCFA/VLCFA synthesis in skin. HEK showed increased mitochondrial mass and membrane potential, but reduced basal and maximal respiratory capacity, consistent with altered mitochondrial function. LCFA uptake increased (BODIPY), with higher SLC27A1/A2 expression and elevated FAO activity. FAO inhibition with etomoxir abrogated butyrate-induced increases in size, granularity, lysosome content, and mitochondrial mass, indicating FAO dependence.
The findings demonstrate that dietary fiber and the SCFA butyrate mitigate allergen-induced AD-like skin inflammation primarily by strengthening the epidermal barrier. Butyrate acts directly on keratinocytes to accelerate terminal differentiation and enhance production of key structural proteins and lipids, thereby reducing allergen ingress and subsequent type 2 immune activation. Immune alterations observed (reduced PD-L2 on APCs, diminished ILC2 and CD4+ T cell responses) are likely secondary to reduced antigen penetration rather than direct immunosuppression, as bypassing the barrier with intradermal allergen delivery eliminated these differences. Mechanistically, at physiologically relevant concentrations, butyrate functions as a metabolic substrate in keratinocytes: it fuels mitochondrial β-oxidation and reshapes lipid metabolism, increases LCFA/VLCFA synthesis and uptake, and drives a mitochondria-dependent differentiation program. Unlike high-dose HDAC inhibition effects reported elsewhere, these barrier-enhancing effects are FAO-dependent and HDACi-independent in this model. The data support a gut–skin axis where dietary fiber and microbial SCFA maintain epithelial barrier integrity, with implications for preventing early allergen sensitization and interrupting the atopic march.
This study establishes that fermentable dietary fiber and gut-derived SCFA—especially butyrate—enhance skin barrier integrity by reprogramming keratinocyte metabolism to promote terminal differentiation and lipid/protein production. Strengthening the stratum corneum limits percutaneous allergen ingress, reduces systemic sensitization, and mitigates AD-like inflammation. The work highlights FAO-driven mitochondrial mechanisms in keratinocytes as therapeutic targets and supports dietary strategies to boost SCFA as preventive or adjunctive measures against AD and related atopic diseases. Future research should evaluate translational relevance in humans, optimal dosing and delivery of SCFA or fiber, long-term safety, interactions with skin and gut microbiota, and potential applications to other epithelial barrier disorders, including exploring SCFA effects on epithelial lipid synthesis in the lung.
- The immune cell landscape was not exhaustively profiled; unassessed populations may contribute to effects, potentially secondary to keratinocyte changes.
- The study relies on murine models and in vitro human keratinocytes; direct clinical efficacy in humans remains to be established.
- Mechanistic divergence from HDACi-mediated effects may depend on SCFA concentration, timing, and cellular context; only selected concentrations (e.g., 0.5 mM butyrate, 0.5 mM valproate) were tested.
- Experimental design lacked randomization and blinding; although group variances were similar and statistics appropriate, potential bias cannot be fully excluded.
- The model uses repeated exposure to protease-active HDM allergens on dorsal skin, which may not capture all facets of human AD heterogeneity.
Related Publications
Explore these studies to deepen your understanding of the subject.