Medicine and Health
GlomSpheres as a 3D co-culture spheroid model of the kidney glomerulus for rapid drug-screening
J. Tuffin, M. Chesor, et al.
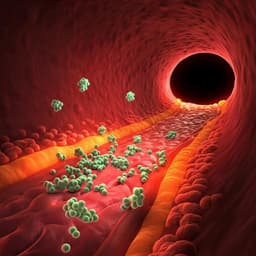
The study addresses the need for more representative, scalable in vitro models of the kidney glomerulus to improve early-stage drug discovery and disease modeling. Conventional 2D monocultures fail to capture the complex cell–cell and cell–matrix interactions, gradients, and architecture of the glomerular filtration barrier, leading to poor physiological relevance and heterogeneous drug responses. While 3D organoids offer improvements, they are often variable, lengthy to produce, and difficult to scale for high-throughput screening. The authors hypothesize that a rapid, reproducible 3D co-culture spheroid model using mature human glomerular cells (podocytes and glomerular endothelial cells) can better recapitulate glomerular structure and molecular phenotype, including deposition of mature GBM components and restoration of key cell-specific markers, and can model disease phenotypes and therapeutic responses suitable for drug screening.
- 2D cultures inadequately reflect tissue microenvironments, failing to reproduce intercellular interactions and ECM context, leading to misleading drug responses.
- Existing 3D models are often scaffold-based (less adaptable for miniaturization/high throughput) or rely on self-aggregation, frequently focused on tumor systems or stem cell-derived organoids. Kidney organoids from iPSCs can generate glomerular structures and podocytes with screening potential but suffer from long protocols and phenotypic variability, limiting reproducibility and throughput.
- Conditionally immortalised human podocytes, GEnCs, and mesangial cells are valuable but are typically used in 2D monoculture, with podocytes showing phenotypic drift.
- There is a recognized need for consistent, scalable in vitro models to study glomerular diseases (e.g., immune-mediated nephrotic syndrome) and to reduce reliance on low-throughput animal models during early drug development.
- Cell lines: Conditionally immortalised human podocytes and glomerular endothelial cells (GEnCs); stable GFP-actin podocytes and mCherry-actin GEnCs generated; podocin-mutant (PM) podocytes used for screening assays. Proliferation at 33±1°C; differentiation at 37°C for 10 days. 2D co-culture at 1:1 on plastic.
- GlomSphere formation: Magnetic spheroid bioprinting (Nano3D Biosciences). For co-culture, form a core spheroid of 5000 GEnCs for 1 h at 33°C, then add 5000 podocytes to wrap the periphery using a 96-magnet MagDrive; thermoswitch to 37°C and differentiate for 10 days. Monoculture spheroids formed with 10,000 cells per well. Magnetic nanoparticles remain bound and are inert/non-fluorescent.
- Experimental design: • Self-organization assessed in mixed spheroids (cells self-organize to GEnC core and podocyte periphery within 72 h). • ECM deposition and GBM maturation assessed by IF (whole-mount and paraffin sections) for collagen IV (pan, a1, a3), laminin a5, and fibronectin, with quantification of mean fluorescence intensity. • Ultrastructure by SEM and TEM to evaluate podocyte foot-process interdigitation, vessel-like protrusions, and deposition of fibrillar collagen IV at podocyte–endothelial interfaces. • Marker expression: Western blots for podocalyxin and PECAM-1 using human glomerular lysate as positive control; IF localization. QPCR for nephrin and podocin mRNA. • Fibrosis modeling: Treatments for 72 h with TGF-β1 (10 ng/ml) ± Adriamycin (10 nM) to induce podocyte loss and ECM dysregulation; co-treatment with Nintedanib (10 μM) as antifibrotic. • Patient plasma challenge: Incubation for 7 days with 15% plasma from FSGS patients during relapse or remission, and relapse + Nintedanib (10 nM), assessing podocyte retention and collagen IV deposition. • High-throughput screening: 96-well plate GlomSpheres using WT or PM podocytes; daily dosing of candidate compounds (including 407 and derivatives); automated live imaging (In-cell analyser) and quantification of GFP intensity and podocyte surface coverage at day 5; comparison to standard 2D podocyte adhesion assay.
- Imaging: Confocal, widefield, lightsheet microscopy; SEM and TEM for ultrastructure. Quantification via ImageJ using ROI-based mean fluorescence intensity and thresholded area for podocyte coverage.
- Molecular assays: Western blot from pooled spheroids (192/well plates combined); QPCR from pooled spheroids with specified primers.
- Statistics: GraphPad Prism; one-way ANOVA with Tukey's multiple comparisons; details and n values in figure legends. Patient plasma sourced with ethical approval and handled under controlled conditions.
- 3D organization and ECM deposition: • GlomSpheres form a GEnC core wrapped by podocytes over 10 days; collagen IV localizes primarily at the podocyte/GEnC interface. • Fibronectin is present extracellularly and enriched at the interface.
- GBM maturation switch: • Collagen IV a1 expression showed no significant difference between monoculture and co-culture (one-way ANOVA P=0.2209). • Collagen IV a3 (mature) significantly increased in GlomSpheres vs podocyte or GEnC monocultures: fluorescence ~44±7 vs ~23±4 and ~24±3; Tukey ****P<0.0001. Western blot densitometry: GlomSphere ~16421±2475 vs podocyte ~360±186 and GEnC ~332±92; ****P<0.0001. • Laminin a5 absent/weak in monocultures but strongly deposited in GlomSpheres: ~47±8 vs ~11±0.5 and ~14±2; ****P<0.0001.
- Ultrastructure: • SEM/TEM show podocyte foot process interdigitation; vessel-like protrusions occasionally observed and PECAM-1 positive; fibrillar collagen IV deposited between neighboring podocytes and endothelial cells (tri-layer structure reminiscent of GBM).
- Restoration of cell-specific markers: • Podocalyxin: absent in 2D lysate, upregulated in GlomSpheres (~6-fold±0.3); glomerular lysate ~10-fold; ****P<0.0001. • PECAM-1: weak in 2D, significantly increased in GlomSpheres approaching glomerular levels (~2.5-fold±0.5); ***P=0.0006. IF shows podocalyxin at periphery (podocytes) and PECAM-1 centrally (GEnCs). • Nephrin mRNA: ~600-fold increase in GlomSpheres vs 2D; **P=0.0092. • Podocin mRNA: ~30,000-fold increase in GlomSpheres vs 2D; ****P<0.0001.
- Induced disease phenotypes and modulation: • TGF-β1 (10 ng/ml) + Adriamycin (10 nM), 72 h: marked podocyte loss (GFP MFI untreated ~87±9 vs ~19±3; ****P<0.0001) and coverage (~41% vs ~2.5%). Nintedanib (10 μM) co-treatment improved podocyte retention (MFI ~39±6; coverage ~10.5%). Collagen IV fluorescence reduced vs untreated under these conditions. • TGF-β1 alone (10 ng/ml), 72 h: increased collagen IV deposition (~36±5 vs ~69±22; ***P=0.0003), attenuated by Nintedanib (~38±8; ***P=0.0006); podocyte loss not significant across conditions.
- Patient plasma challenge: • FSGS relapse plasma (7 days, 15%) reduced podocyte attachment vs remission: GFP intensity ~9±1 vs ~17±2; coverage ~29% vs ~57%; ****P<0.0001 for both. Nintedanib improved podocyte retention vs relapse (intensity ~13±2; coverage ~46%; ****P<0.0001). • Collagen IV increased in relapse vs remission (~100±20 vs ~61±15; **P=0.0014). Relapse+Nintedanib yielded even higher collagen IV (~129±51) than relapse (*P=0.0401) and remission (****P<0.0001), indicating altered deposition pattern and lack of antifibrotic effect on ECM in this context.
- Screening utility: • Automated 96-well imaging demonstrated greater dynamic range vs 2D adhesion assay. WT podocytes attached better than podocin-mutant; several compounds (e.g., series derived from compound 407 such as 53) rescued podocyte retention toward WT levels in 3D, with more compounds reaching statistical significance compared to 2D.
GlomSpheres restore aspects of glomerular tissue architecture and molecular phenotype lost in 2D culture, including maturation of GBM components (collagen IV a3 and laminin a5) and robust expression of podocyte and endothelial markers (podocin, nephrin, podocalyxin, PECAM-1). Ultrastructural features such as podocyte interdigitating foot processes and vessel-like PECAM-1 positive structures suggest a more physiologically relevant microenvironment and signaling, likely supporting slit diaphragm function. The model can isolate and independently examine two central elements of glomerulosclerosis—podocyte detachment and ECM dysregulation—by applying TGF-β1 with or without Adriamycin, and it enables assessment of therapeutic modulation by Nintedanib. Exposure to patient relapse plasma reproduces clinically relevant podocyte injury and ECM changes distinct from single-factor stimuli, with partial protection by Nintedanib for podocyte retention but not ECM. The rapid, scalable imaging workflow shows improved sensitivity over 2D adhesion assays, enhancing identification of efficacious compounds (e.g., derivatives of 407). Collectively, GlomSpheres provide a more representative and high-throughput-compatible in vitro platform to study glomerular pathology and to screen anti-fibrotic and podocyte-protective agents.
The study introduces GlomSpheres, a robust and scalable 3D co-culture spheroid model of human glomerulus that rapidly recapitulates key structural and molecular hallmarks, including a mature GBM protein profile and restoration of podocyte and endothelial markers. The model supports mechanistic studies of glomerulosclerosis by independently modeling podocyte loss and ECM dysregulation and demonstrates pharmacological modulation with Nintedanib. It also enables medium/high-throughput drug screening with improved dynamic range relative to 2D assays and identifies compounds that rescue podocyte adhesion in a podocin-mutant context. Future work may incorporate additional glomerular cell types (e.g., mesangial cells), perfusion/flow to support capillary maturation, and functional readouts of filtration to further enhance physiological relevance.
- Absence of mesangial cells, which provide matrix components, signaling, and structural support for capillaries.
- Lack of perfusion/flow; while primitive vascularization is observed, true capillary architecture and function likely require flow.
- The model does not currently assess glomerular filtration function; modifications to enable functional assays may reduce scalability.
- Variability in patient-derived plasma contents and lack of healthy control plasma due to clinical constraints on plasmapheresis.
- Use of conditionally immortalised cell lines may not capture all aspects of primary cell behavior despite demonstrated restoration in 3D.
Related Publications
Explore these studies to deepen your understanding of the subject.