Medicine and Health
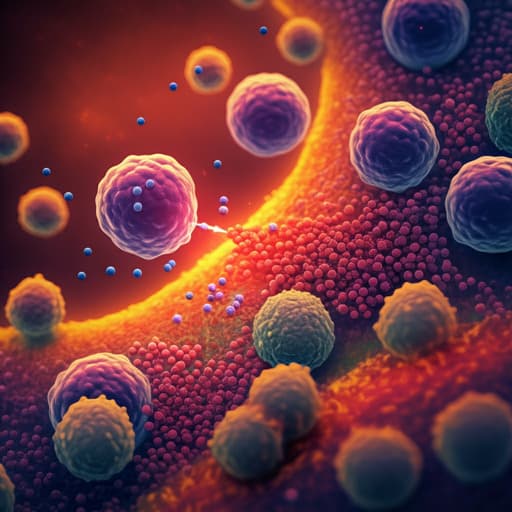
Efficacy and safety of nanoparticle albumin-bound paclitaxel monotherapy after immune checkpoint inhibitor administration for advanced non-small cell lung cancer: A multicenter Phase 2 clinical trial
T. Sonoda, Y. Umeda, et al.
This Phase 2 study by Tomoaki Sonoda and colleagues investigates the efficacy and safety of nab-paclitaxel in advanced non-small cell lung cancer patients after PD-(L)1 inhibitor failure. With an impressive objective response rate of 55.2% and median overall survival of 11.9 months, the findings promise new hope in treating this challenging condition.
Related Publications
Explore these studies to deepen your understanding of the subject.