Medicine and Health
Effect of Neutralizing Monoclonal Antibody Treatment on Early Trajectories of Virologic and Immunologic Biomarkers in Patients Hospitalized With COVID-19
T. O. Jensen, G. A. Grandits, et al.
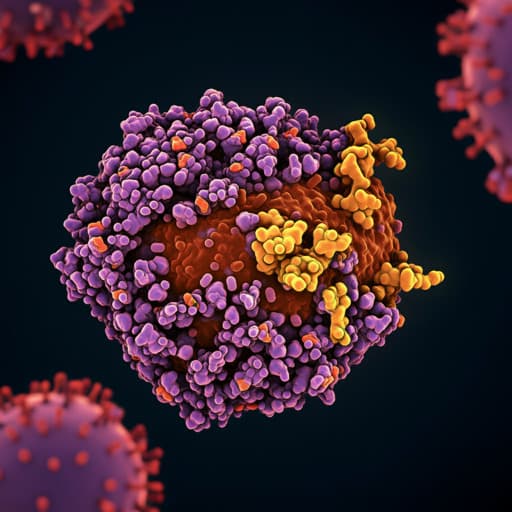
Neutralizing monoclonal antibodies (nmAbs) have not shown consistent clinical benefit in hospitalized patients with COVID-19 despite demonstrated antiviral activity in other settings. Identifying which hospitalized patients might benefit and understanding how virologic and immunologic biomarkers evolve after nmAb therapy remain open questions. Prior analyses suggested potential benefit in subgroups with low baseline antispike antibody titers, high plasma SARS-CoV-2 nucleocapsid antigen (N-Ag), or higher levels of respiratory support. The TICO/ACTIV-3 platform conducted randomized, blinded, placebo-controlled trials of several nmAbs in hospitalized patients receiving standard of care, including remdesivir. This study aimed to characterize early trajectories (days 0–5) of virologic (plasma N-Ag) and immunologic (anti-nucleocapsid and anti-spike neutralizing activity) biomarkers, as well as inflammatory markers (CRP, IL-6, D-dimer), following nmAb treatment versus placebo, to inform treatment strategies at hospital admission and future trial design.
The study references multiple randomized trials and platform studies evaluating nmAbs in hospitalized COVID-19 patients (ACTIV-3 TICO trials of bamlanivimab, sotrovimab, amubarvimab-romlusevimab, tixagevimab-cilgavimab) and the RECOVERY trial of casirivimab–imdevimab. Prior work identified associations between plasma viral markers (RNAemia, N-Ag) and disease severity/outcomes, and suggested subgroup-dependent responses to nmAbs (e.g., anti-spike seronegative, high antigen levels, higher oxygen support). Standard-of-care therapies, including remdesivir and immunomodulators (systemic corticosteroids, IL-6 inhibitors, baricitinib), are also discussed in the context of evolving inpatient COVID-19 management. The study builds on these findings by providing detailed, placebo-controlled trajectories of biomarkers over the first 5 days after treatment.
Design and setting: Analysis of four international, blinded, randomized, placebo-controlled TICO/ACTIV-3 trials of nmAbs in hospitalized adults with laboratory-confirmed SARS-CoV-2 infection, symptom duration ≤12 days, and no organ failure or major extrapulmonary manifestations. Enrollment occurred from 5 August 2020 to 30 September 2021 across 108 sites in Denmark, Greece, Poland, Uganda, Singapore, Spain, Switzerland, the United Kingdom, and the United States. Interventions: nmAbs evaluated included bamlanivimab (Eli Lilly), sotrovimab (Vir Biotechnology/GlaxoSmithKline), amubarvimab–romlusevimab (Brii Biosciences), and tixagevimab–cilgavimab (AstraZeneca). Participants were randomized to active nmAb or placebo. Remdesivir was provided as standard of care unless contraindicated; systemic corticosteroids and other treatments were used per local practice. Participants: Hospitalized adults not requiring invasive mechanical ventilation; patients on no oxygen or conventional oxygen were eligible for all trials; bamlanivimab and tixagevimab–cilgavimab trials also enrolled those on high-flow nasal oxygen (HFNO) or noninvasive ventilation (NIV). Inclusion in this analysis required a baseline (day 0) sample and at least one follow-up sample on days 1, 3, or 5 for the biomarker of interest. Laboratory measurements: Centralized, blinded assays measured plasma nucleocapsid antigen (N-Ag; Quanterix SARS-CoV-2 N Protein Antigen assay; LOD 3 ng/L), anti-nucleocapsid total antibody (BioRad Platelia SARS-CoV-2 Total Ab; signal-to-cutoff ratio; positive if >1), anti-spike neutralizing activity (GenScript cPass surrogate neutralization; percent inhibition; positive if ≥30%), CRP and IL-6 (electrochemiluminescence, Meso Scale Discovery), and D-dimer (enzyme-linked fluorescent assay, VIDAS; ULN: CRP 10 mg/L, IL-6 2 ng/L, D-dimer 0.5 mg/L). Variant assessment: Baseline midturbinate swabs underwent RT-PCR targeting spike NTD and N gene control for Delta detection for participants enrolled after 1 May 2021; earlier enrollees were considered non-Delta. Whole-genome sequencing confirmed RT-PCR results (99.9% concordance; n = 811). Statistical analysis: To account for changing randomization proportions and shared placebo across overlapping trials, five strata were defined based on nmAb availability at randomization; pooled nmAb vs placebo comparisons were stratified by this variable. For individual nmAb vs contemporaneous placebo comparisons, approximately equal numbers were achieved. Biomarkers with skewed distributions (N-Ag, CRP, IL-6, D-dimer) were log-transformed; analyses reported geometric means and geometric mean ratios (GMRs). Anti-N and anti-S neutralizing activity were analyzed on the original scale (means and mean differences). Linear mixed models estimated longitudinal treatment effects over days 1, 3, and 5, with fixed effects for treatment, visit (categorical), baseline oxygen requirement (pulmonary ordinal scale), baseline biomarker value, and random subject intercepts; pooled analyses also adjusted for study stratum. Treatment-by-day interactions tested variation in effects over time. Prespecified subgroup analyses assessed effect modification by age, sex, comorbidities, viral variant, symptom duration, pulmonary ordinal scale, baseline N-Ag, anti-N serostatus, anti-S serostatus, and vaccination status; significance threshold set at P ≤ .01 for subgroups. Clinical outcome: Day 5 pulmonary ordinal scale (7-point) analyzed via proportional odds models to estimate common odds ratio for better category with nmAb vs placebo. Nominal P ≤ .05 considered significant (except subgroups). Analyses used SAS 9.4 and R 4.1. Ethics: Written informed consent obtained from each participant or legally authorized representative.
- Participants: 2149 participants with baseline and ≥1 follow-up measurement (Aug 2020–Sep 2021). Median age 57 years (IQR 46–68), 58% male, 83.4% with ≥1 chronic illness, 8.8% fully vaccinated. Median symptom duration 8 days (IQR 6–10). At enrollment, 74.3% required oxygen; 9.2% on HFNO/NIV. Systemic corticosteroids used in 68.2%. Remdesivir use increased from 60.3% pre-enrollment to 92.6% post-randomization. Delta variant in 30.9%.
- Baseline biomarkers: Plasma N-Ag detected in 94.6%. Anti-N Ab positive in 61.9% (median S/C 2.4). Anti-S neutralizing positive in 49.6% (mean 38.1% inhibition). Median CRP 31 mg/L, IL-6 6 ng/L, D-dimer 0.9 mg/L.
- Plasma N-Ag trajectory: Geometric mean levels (nmAb vs placebo): baseline 847 vs 844 ng/L; day 1 442 vs 474 ng/L; day 3 43 vs 62 ng/L; day 5 12 vs 15 ng/L. Adjusted treatment effect averaged over days 1, 3, 5: GMR 0.80 (95% CI 0.73–0.88; P < .001), indicating 20% lower N-Ag with nmAb. Steeper decline over time with nmAb (treatment-by-day interaction P < .001). Among individual agents, bamlanivimab showed the smallest effect; differences between agents were not statistically significant (P = .64).
- Anti-N Ab trajectory: Increased over time in both groups with no significant differences at days 1, 3, or 5, nor averaged across follow-up (no treatment-by-time interaction), indicating no blunting of endogenous anti-N response by nmAb.
- Anti-S neutralizing activity: Marked immediate increase by day 1 in nmAb recipients, consistent with exogenous anti-spike antibodies; placebo showed smaller linear increases. Sotrovimab produced a lower measured increase, consistent with assay target characteristics.
- Inflammatory biomarkers: CRP declined over time; IL-6 and D-dimer showed less pronounced declines. No statistically significant differences between nmAb and placebo for CRP, IL-6, or D-dimer; no treatment-by-time interactions.
- Subgroups: Treatment effects were homogeneous across subgroups (age, sex, comorbidities, variant, symptom duration, oxygen support level, baseline N-Ag, anti-N/anti-S serostatus, vaccination). Most subgroups showed significant N-Ag reduction with nmAb but no differences in other biomarkers. No significant interactions detected.
- Clinical outcome: No effect on day 5 pulmonary ordinal scale in the total cohort (common odds ratio 1.01; 95% CI 0.87–1.18) or in subgroups.
nmAb treatment in hospitalized COVID-19 patients receiving remdesivir was associated with a modest but statistically significant antiviral effect, reflected by lower plasma nucleocapsid antigen levels and a steeper decline over the first 5 days compared with placebo. However, this antiviral signal did not translate into reductions in systemic inflammatory biomarkers (CRP, IL-6, D-dimer) or improved early clinical status (day 5 pulmonary ordinal scale). The absence of endogenous anti-nucleocapsid antibody blunting alleviates prior concerns that exogenous anti-spike nmAbs might suppress humoral responses. The uniformity of effects across key subgroups, including patients anti-spike seronegative at baseline and those requiring HFNO/NIV, suggests that nmAb efficacy signals on viral antigenemia are broadly consistent but insufficient to impact early clinical trajectories in this inpatient population. Two nonexclusive interpretations emerge: (1) nmAbs, layered onto remdesivir, may not provide sufficient additional antiviral potency to alter the short-term inflammatory and clinical course; or (2) once hospitalized, disease progression is driven predominantly by dysregulated host inflammation rather than ongoing viral replication, limiting the clinical impact of further antiviral augmentation at this stage. Earlier administration in the disease course might be necessary to observe downstream anti-inflammatory and clinical benefits. Alternatively, more potent or mechanistically distinct antivirals or enhanced immunomodulatory strategies could be required to influence outcomes in hospitalized patients.
In a large, placebo-controlled analysis across four TICO/ACTIV-3 trials, neutralizing monoclonal antibody therapy in hospitalized COVID-19 patients produced a modest antiviral effect measured by plasma nucleocapsid antigen without affecting systemic inflammation or early clinical status, and without impairing endogenous anti-nucleocapsid antibody responses. These findings argue against meaningful early clinical benefit of current nmAbs in this inpatient setting. Future research should evaluate earlier administration, more potent/different antiviral mechanisms, and optimized immunomodulatory approaches, and assess generalizability in contemporary, highly vaccinated populations with Omicron-lineage infections.
- Plasma nucleocapsid antigen, while correlated with severity and outcomes, may not specifically reflect ongoing viral replication.
- Pooled analysis across four different nmAb agents assumes similar effects and may mask agent-specific differences.
- Universal/background use of remdesivir could attenuate incremental antiviral effects attributable to nmAbs.
- Generalizability to contemporary settings with high vaccination rates and Omicron sublineages is uncertain.
- Multiple outcomes and subgroup analyses were exploratory without formal adjustment for multiplicity (increased type I error risk).
Related Publications
Explore these studies to deepen your understanding of the subject.