Medicine and Health
A first-in-class leucyl-tRNA synthetase inhibitor, ganfeborole, for rifampicin-susceptible tuberculosis: a phase 2a open-label, randomized trial
A. H. Diacon, C. E. B. Iii, et al.
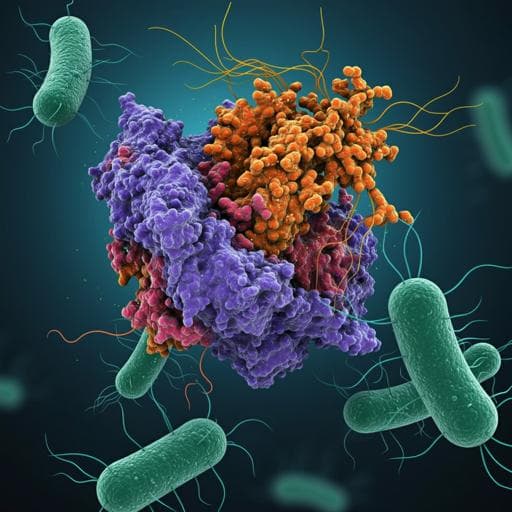
Tuberculosis (TB) remains a leading global cause of death with 1.6 million deaths in 2021, and drug-resistant TB threatens control efforts. Standard therapy for drug-susceptible TB (rifampicin, isoniazid, pyrazinamide, ethambutol) requires 6 months and has tolerability and resistance challenges. New agents are needed that can shorten therapy, improve tolerability, and retain activity against resistant strains. GSK3036656 (ganfeborole) is a novel benzoxaborole that inhibits Mycobacterium tuberculosis leucyl-tRNA synthetase, showing potent in vitro activity against drug-susceptible, multidrug-resistant and extensively drug-resistant strains, and in vivo efficacy in animal models. A phase 1 study showed acceptable safety and pharmacokinetics, and translational PK/PD modeling predicted early bactericidal activity (EBA) at clinical doses. This phase 2a trial aimed to evaluate the EBA, safety, and pharmacokinetics of ganfeborole monotherapy at multiple doses in untreated, rifampicin-susceptible pulmonary TB, with exploratory PET/CT and transcriptional profiling analyses.
The paper situates ganfeborole among recent TB drug advances (bedaquiline, delamanid, pretomanid) and highlights ongoing uncertainties regarding optimal dosing, combinations, and treatment shortening with these agents. It notes limitations of second-line regimens (cost, tolerability, pill burden, toxicity) and the emergence of strains resistant to all available drugs. Prior preclinical work demonstrated ganfeborole’s potency against M. tuberculosis in vitro and in animal models (mouse, marmoset), and a first-in-human study established tolerability and PK. EBA as an early clinical efficacy measure is well established and correlates with microbiological endpoints such as CFU reduction and increased time to positivity in culture. The authors reference PET/CT imaging as a modality to monitor lesion-level treatment responses over short intervals and transcriptomic analyses to understand immunologic correlates of response.
Design: Single-center, open-label, randomized, sequential cohort phase 2a trial (TASK clinical research center, Cape Town, South Africa), conducted March 2019–December 2021; ClinicalTrials.gov NCT03557281. Participants were recruited into four cohorts and randomized 3:1 to ganfeborole or standard of care (SOC). The study was designed for within-cohort change-from-baseline analyses and not powered for between-group comparisons. Participants: Male, 18–65 years, 40–90 kg, new untreated rifampicin-susceptible pulmonary TB; chest X-ray consistent with TB and microbiologic confirmation; normal troponin; creatinine clearance ≥75 ml/min; acceptable echocardiogram. Key exclusions included extrapulmonary TB, QTcF >450 ms, relevant drug allergies, vitiligo, HIV infection with CD4+ <350 cells/µl, recent antiretroviral/antifungal therapy, or AIDS-defining illness. PET/CT subgroup required age ≥25 years. Randomization and masking: Within each cohort, 3:1 randomization to ganfeborole or SOC using permuted blocks; open-label for participants/investigators; laboratory staff measuring CFU and TTP were blinded to allocation. Interventions: Ganfeborole once daily (QD) for 14 days with loading dose on day 1, followed by maintenance doses days 2–14. Sequential cohorts received: 5 mg (15 mg loading), 15 mg (30 mg loading), 30 mg (75 mg loading), and finally 1 mg (3 mg loading) to delineate dose-response. SOC (Rifafour e-275 or generic alternative) was weight-adjusted per South African guidelines (rifampicin 150 mg, isoniazid 75 mg, pyrazinamide 400 mg, ethambutol 275 mg per tablet) and served as a benchmark for assay reproducibility. All participants initiated SOC on day 15 after completing study treatment. Assessments: Serial overnight sputum collections daily from baseline to day 4 and on alternate days from day 6 to day 14. Primary endpoint: EBA CFU0–14, the mean daily rate of change in log10 CFU/ml from baseline to day 14. Secondary EBA endpoints: CFU0–2, CFU2–14; TTP0–14, TTP0–2, TTP2–14. Safety: adverse events (AEs), labs, vital signs, ECGs, physical exams, echocardiograms through day 28 follow-up. Pharmacokinetics (PK): pre-dose samples days 12–13 and serial sampling day 14 for plasma ganfeborole concentrations; non-compartmental analysis of AUC0–24, Cmax, tmax. Exploratory: PET/CT at baseline and day 14 in 1 mg and 30 mg cohorts; computational segmentation and registration with voxel-based analysis of lesion features (volume, total glycolytic activity [TGA], total associated mass [TAM]) stratified by density/uptake categories; correlation with whole-blood RNA sequencing (CIBERSORT for cell fractions; gene set enrichment analyses). Populations: Safety population: all randomized participants receiving ≥1 dose. Efficacy population: safety population with ≥2 evaluable overnight sputum samples (including baseline). PK population: safety population receiving ganfeborole with ≥1 evaluable PK sample. Statistics: Mixed model repeated measures for primary and secondary EBA endpoints including covariates for treatment, time, BMI, treatment-by-time; baseline CFU or TTP as covariates in models for days 2–14; mean daily rate of change with 95% CIs reported. A bilinear Bayesian regression model was additionally fitted for CFU and TTP from baseline to day 14. No formal hypothesis testing; sample size informed by simulations showing high probability (>90%) to detect a negative mean change with n≈9–15 per group given assumed effect size and variability. Safety summarized descriptively. PET/CT analyses blinded to dose; manual and computational segmentation employed. RNA analyses used CIBERSORT and KEGG pathway-based enrichment.
Participants: 168 screened; 76 enrolled and randomized; 75 treated (SOC n=18; ganfeborole 1 mg n=9; 5 mg n=17; 15 mg n=16; 30 mg n=15). Completion rates: SOC 100% (18/18); ganfeborole 1 mg 89% (8/9); 5 mg 82% (14/17); 15 mg 88% (14/16); 30 mg 87% (13/15). All participants were male and Black; baseline characteristics (age, BMI) were similar across groups. Efficacy (EBA): Decreases in log10 CFU/ml and increases in TTP were observed for ganfeborole 5–30 mg and SOC over 14 days; 1 mg showed minimal or no EBA.
- EBA CFU0–14 (mean daily change in log10 CFU/ml; estimate [95% CI]): SOC −0.199 [−0.224, −0.174]; 1 mg −0.017 [−0.052, 0.019]; 5 mg −0.092 [−0.119, −0.066]; 15 mg −0.092 [−0.120, −0.065]; 30 mg −0.138 [−0.167, −0.109].
- EBA TTP0–14 (mean daily change in log10 h; estimate [95% CI]): SOC 0.025 [0.023, 0.027]; 1 mg 0.000 [−0.003, 0.003]; 5 mg 0.015 [0.012, 0.017]; 15 mg 0.021 [0.018, 0.023]; 30 mg 0.022 [0.019, 0.024]. Early (0–2 days) and late (2–14 days) intervals:
- EBA CFU0–2: SOC −0.598 [−0.756, −0.440]; 1 mg 0.250 [0.037, 0.463]; 5 mg −0.153 [−0.311, 0.005]; 15 mg −0.055 [−0.220, 0.109]; 30 mg −0.040 [−0.209, 0.129].
- EBA CFU2–14: SOC −0.162 [−0.195, −0.129]; 1 mg −0.037 [−0.083, 0.009]; 5 mg −0.080 [−0.114, −0.046]; 15 mg −0.086 [−0.122, −0.050]; 30 mg −0.129 [−0.167, −0.092].
- EBA TTP0–2: SOC 0.105 [0.092, 0.118]; 1 mg −0.003 [−0.022, 0.016]; 5 mg 0.021 [0.007, 0.035]; 15 mg 0.032 [0.018, 0.046]; 30 mg 0.066 [0.051, 0.081].
- EBA TTP2–14: SOC 0.017 [0.015, 0.019]; 1 mg 0.001 [−0.002, 0.004]; 5 mg 0.013 [0.011, 0.015]; 15 mg 0.017 [0.015, 0.020]; 30 mg 0.016 [0.014, 0.019]. Safety: AE rates comparable across groups; all AEs grade 1–2; no serious AEs. Any AE: SOC 78%, 1 mg 78%, 5 mg 82%, 15 mg 94%, 30 mg 60%. Drug-related AEs: SOC 28%, 1 mg 44%, 5 mg 24%, 15 mg 31%, 30 mg 13%. AEs leading to treatment withdrawal: 1 participant each in 5 mg (day 11, hemoptysis) and 15 mg (day 10, suspected disease progression). Most common AEs with ganfeborole: hemoptysis (n=8 overall) and pruritus (n=7). No dose-dependent increase in drug-related AEs observed. Pharmacokinetics (Day 14, PK population): Rapid absorption with median tmax ~1.0–2.5 h. Geometric mean (CVb%) AUC0–24 (ng·h/ml): 1 mg 282.1 (25.8%); 5 mg 1,497.1 (12.4%); 15 mg 4,493.9 (12.5%); 30 mg 11,540.0 (17.8%). Cmax (ng/ml): 1 mg 16.93 (23.7%); 5 mg 94.60 (24.7%); 15 mg 291.41 (18.9%); 30 mg 705.24 (20.2%). Approximate dose proportionality from 1–15 mg; more than dose-proportional increase in exposure at 30 mg. Exploratory PET/CT (post hoc): 19 participants (1 mg n=6; 30 mg n=13) with baseline and day 14 scans. Ganfeborole 30 mg associated with reductions in lesion-associated radiodensity (TAM) across participants and reductions in total glycolytic activity (TGA) in 11/13 participants; 1 mg showed little change or worsening. Greatest impact at 30 mg in ‘hot’ lesions (SUVmean >2) including consolidations/infiltrates; appreciable impact on cavity walls. Qualitatively similar lesion feature responses to rifampicin and moxifloxacin in prior EBA imaging studies. Transcriptional profiling: At day 14, ganfeborole 30 mg showed differential expression involving neutrophil degranulation/activation pathways and increased CD8 T cell activity versus baseline and versus 1 mg; 1 mg showed higher neutrophil and plasma cell activity at day 14 relative to 30 mg. Correlation of blood transcriptional changes with PET/CT responses suggested association with neutrophil-dominated modules.
Daily ganfeborole at 5–30 mg demonstrated early bactericidal activity over 14 days in rifampicin-susceptible pulmonary TB, with the strongest EBA at 30 mg and minimal activity at 1 mg. SOC behaved as expected, supporting assay validity. Safety was acceptable with only mild-to-moderate AEs and no serious AEs, and no clear dose-dependent increase in drug-related events. PK showed rapid absorption and approximately dose-proportional exposure up to 15 mg with supra-proportional exposure at 30 mg, consistent with prior phase 1 data. Post hoc PET/CT analyses indicated that ganfeborole particularly affected metabolically active (‘hot’) lesion components, including infiltrates and cavity walls, and transcriptomic profiles suggested modulation of neutrophil-related pathways and increased CD8 T cell activity at effective dosing. Integrating PK/PD and in silico simulations from the broader ganfeborole program, the authors propose 20 mg QD as an optimal dose for future combination studies, balancing efficacy and exposure. Overall, the findings support ganfeborole’s potential role as a component of novel, pan-TB regimens with low drug–drug interaction potential.
Ganfeborole, a first-in-class leucyl-tRNA synthetase inhibitor, showed measurable early bactericidal activity at 5–30 mg QD over 14 days, with the greatest effect at 30 mg, and an acceptable safety and tolerability profile in adult males with rifampicin-susceptible pulmonary TB. Exploratory imaging and transcriptomics align with antimicrobial effects in highly active lesion compartments and neutrophil-associated pathways. These results support further evaluation of ganfeborole in longer-duration, combination regimens, dose optimization (with 20 mg QD proposed for future trials), and studies including diverse populations and drug-resistant TB.
- No placebo/negative control arm due to ethical constraints; SOC used as a benchmark but not directly comparable to ganfeborole monotherapy, and no formal between-arm statistical comparisons were performed.
- Short treatment duration (14 days) and monotherapy; long-term efficacy and sterilizing activity require longer combination studies.
- Population limited to males; subsequent studies including females are planned.
- All participants were Black and from a single South African center, which may limit generalizability; however, prior PK analyses did not identify race as a significant covariate.
- PET/CT and transcriptomic analyses were post hoc and conducted in small subsets, limiting inference and requiring confirmation.
- Data generated in drug-susceptible TB; applicability to drug-resistant TB regimens needs direct evaluation.
Related Publications
Explore these studies to deepen your understanding of the subject.